Introduction
Patients are more concerned about their aesthetics that has led to the development of tooth colored, non-metallic restorations such as direct composite restorations and indirect composite restorations.1 Dental composite resins initially were used in anterior teeth region. Later with the advent of technology and material science, the physical and mechanical properties of resin-based composites have been considerably improved their clinical applications. 2
Although the use of resin composites has grown considerably, many drawbacks are associated with their use in the posterior region, such as polymerization shrinkage, gap formation, occlusal wear, and color instability. 3, 4 To overcome these clinical challenges, manufacturers developed materials and techniques for indirect construc- tion of resin composite restorations.4
Indirect technique by secondary/additional curing extra orally using light and heat, has resulted in higher rate of degree of conversion, reduction in the amount of intra oral polymerization shrinkage, better control of contour and contacts, marginal adaptations, enhanced physical properties, improved polishability, less water solubility. 5, 6
The only polymerization shrinkage that is unavoidable is the shrinkage due to resin cement which is used for the luting of indirect restorations. 5 Several types of resin cements are available to cement the indirect restorations. The resin cements differ from each other by pre- treatment of tooth surface prior to application of resin cements, i.e., etch and rinse, self- etch adhesive, self-adhesive resin cements. 7
A variety of factors can influence the performance of luting material, including the clinical scenario, the polymerization method, degree of conversion, the physical/chemical properties and the biological aspect regarding the pulp response. 8 Despite the innovations to enhance the clinical success of numerous restorative procedures, micro leakage persists as one of the main cause of restoration failure.
Micro leakage can cause a variety of adverse effects, such as secondary caries, high sensitivity of the restored tooth, and interfacial staining leading to pulp pathology. Micro leakage most commonly occurs, when the gingival margin of any restoration is placed below the cemento- enamel junction because bonding to dentin is less predictable than enamel due to its complex pattern and lower mineral content. 9
Very few articles have studied comparing self-etch primer adhesives and self-adhesive resin cements at different storage periods. Therefore this study assessed the microleakage in composite inlays by using Multilink N and Multilink speed at 24 hours and 2 months storage period.
The null hypothesis is that 1. There is no significant difference in microleakage between tested materials. 2. Storage period does not influence the microleakage of resin cements.
Materials and Methods
Freshly extracted eighty premolar teeth were taken for the study which were free from caries, hypoplastic defects and cracks on visual examination. All teeth were cleaned to remove surface debris and calculus by ultrasonic scaler. The teeth were disinfected with 0.1% thymol solution and randomly divided into eight groups of ten (n=10), each based on the storage time, placement of classII cavity gingival margin and the type of luting agent used. Teeth were mounted.
Cavity preparation
Standardized class II inlay box cavities were prepared on each tooth using high speed hand piece along with air and water spray. The dimensions of each cavity was 2mm mesiodistally and 4mm buccolingually. Out of 80 samples, in 40 samples, the gingival margin was kept 1mm coronal to CEJ i.e supragingival, and for the remaining 40 samples, the gingival margin was kept 1mm apical to CEJ i.e subgingival.
Following that, separating medium was applied, composite (Te – economy plus, Ivoclar Vivadent AG, Shaan, Liechtenstein) was placed incrementally and cured initially (40 sec) using halogen light curing unit (spectrum 800, densply sirona) with an intensity 650 mW/cm2. Then, the composite inlays were removed from the teeth and post cured in polymat light curing unit (Delta Dental). Bonding surface of the inlays were sandblasted using intra oral microetcher device and 50 micron Al2O3 powder for 5 seconds from 5mm distance and 60 PSI pressure. Sandblasted surfaces were irrigated with water and air dried.
Teeth are grouped as follows
24 Hours storage Groups
GROUP I – supra gingival cavity margin with Multilink N as a luting agent GROUP II- supra gingival cavity margin with Multilink speed as a luting agent GROUP III- sub gingival cavity margin with Multilink N as a luting agent
GROUP IV- sub gingival cavity margin with Multilink speed as a luting agent
2 Month storage Groups
GROUP V- supra gingival cavity margin with Multilink N as a luting agent
GROUP VI- supra gingival cavity margin with Multilink speed as a luting agent
GROUP VII- sub gingival cavity margins with Multilink N as a luting agent
GROUP VIII- sub gingival cavity margins with Multilink speed as a luting agent
Cementation of inlays
For group I, III,V,VII, the multilink N was used as luting agent for semi indirect inlays. For group II, IV, VI, VIII the multilink speed was used as luting agent for semi indirect inlays.The luting cements were mixed and applied as per the manufacturers instructions.
The inlay was seated into the cavity and excess material was removed with scalers. The margins were light cured for 20 seconds as per the manufacturer’s instructions. Restorations were finished and polished using composite finishing discs (Soflex 3M ESPE, USA).
Groups I to IV were stored for 24 hours at room temperature and groups V to VIII were stored for 2 months at room temperature. The samples were thermocycled using Willytech thermocycler for 500 cycles at 5ºc and 55ºc, with 30 seconds dwell time and 5 seconds transfer time (ISO TR 11450 standard-1994).
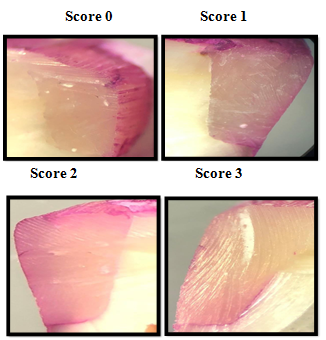
The teeth apices were sealed with flowable composite resin. Two layers of nail varnish was applied to all the tooth surfaces except for about 1mm around the restoration margin. All the samples were then placed in 0.5% basic fuchsin for 24 hours. After dye penetration and irrigation of the teeth, samples were sectioned mesio-distally in vertical plan using a diamond disc in slow speed with water spray. The sections were mounted on slides and the degree of dye penetration was recorded under stereomicroscope with X20 magnification. Leakage was evaluated according to scores mentioned below for the degree of dye penetration
Evaluation criteria
A: Occlusal margin
1 - No microleakage
2 - Microleakage not reaching the DEJ
3 -Microleakage penetration over the DEJ
4 -Microleakage into the dentinal tubule towards the pulp
B: Cervical margin
1 - No microleakage
2 - Microleakage less than half the cervical wall of the cavity
3 - Microleakage penetration through all the cervical wall of the cavity
4 -Microleakage along the cervical or axial wall, into the dentinal tubules
Statistical analysis
Statistical analysis of the data was performed using SPSS 21 IBM. The data regarding the microleakage analyzed with Mann – whitney U test and it was used to determine microleakage between resin cements at cervical margin and occlusal margins. Wilcoxon signed rank test was used to determine microleakage with in the group comparison for 24 hours and 2 months storage period. Probability value (P)<0.005 was considered as significant difference.
Results
There was no statistically significant difference of microleakage values between the two luting cements for a storage period of 24 hours (P=0.067) (Table 1) whereas there was statistically significant difference between them for a storage period of 2 months (P=0.035) for both supra and sub gingival groups seen at the cervical margin. There was no statistically significant difference between two the cements for supra and subgingival groups for the storage period of 24 hours & 2 months when seen at occlusal margin.(Table 2)
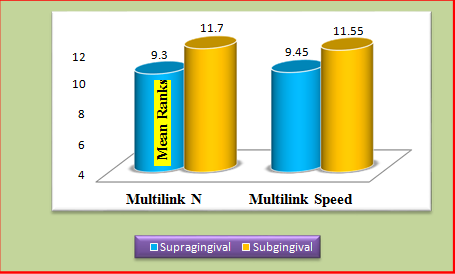
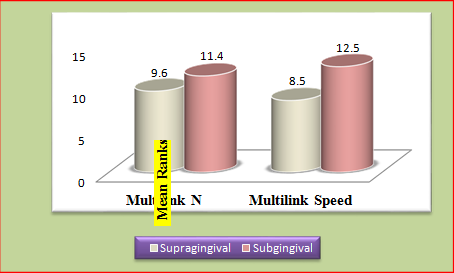
Microleakage comparison between supra and sub gingival groups of multilink n and multilink speed at 24 hrs and 2 moths storage period showed statistically no significant difference.(Table 3, Figure 3, Figure 4)
Table 1
Comparison of the micro leakage at cervical Margin
Table 2
Comparison of the micro leakage at occlusal Margin
Table 3
Microleakage comparison between supra and subgingival groups of Multilink N and Multilink speed at 24 hrs and 2 months storage period
Discussion
The need for an ideal esthetic material for restoring teeth has led to significant advances in both the material and the technical aspect. Resin composites and the acid etch technique represent two such major advances.
Resin composites harden through free radical polymerization of methacrylate groups, that leads to decrease in volume from 1% to 5%, thereby causing polymerization shrinkage.10 The adverse effects of polymerization shrinkage have been reviewed by Soderholm and others, they stated that polymerization shrinkage stresses might produce defects in the interface of composite-dentin, this leads to marginal gap formation, marginal leakage, post-operative sensitivity, recurrent caries and eventually bond failure. Causton and others reported that placement of bonded composite restorations in extracted teeth resulted in a decrease in the distance between cusps (cuspal flexure), which may have resulted in post-operative sensitivity and opened up pre-existing enamel microcracks. 11
In the past, different techniques have been recommended to minimize the effects of polymerization shrinkage such as incremental placement, guided shrinkage technique, soft-start polymerization and pulse delay techniques use of low modulus lining materials, such as glass ionomers cement, resinous liners, new-generation dentin bonding agents and megafillers. Till date, none of the technique or material has been proven to be completely successful in counteracting the ill effects of polymerization shrinkage. One of the main reason for the replacement of direct resin composite restorations is the clinical consequence of the polymerization shrinkage.12
To overcome these limitations, the concept of the heat-treated composite inlay/onlay was developed by Wendt and demonstrated that heat treating at 250°F for seven to eight minutes substantially improved hardness and wear resistance of the resins. This had led to the evolution of post-cure units. 13
Recent post-cure units, along with heat and pressure, use an additional light source for post curing the resin composites. The fabrication method of resin inlay can be divided into two types; Combined direct-indirect/semi-direct technique & Indirect technique.
In the direct-indirect technique, the fabrication of resin composite inlay is done directly on prepared tooth surface in the mouth, removed and cured in a curing oven. In the indirect technique, the impression of the prepared tooth is taken and resin composite inlay is fabricated on a die. The advantage of the direct- indirect technique is that it can be done in single sitting, and the errors that occur during impression making and die fabrication can be avoided. In the present study semi-direct method was selected.
The long-term clinical success of indirect restorative procedure strongly depends on the cementation system and its sealing ability. Various types of resin cement are available to cement an indirect restoration. When compared with traditional resin luting materials, a resin luting material that does not require the etching and bonding steps could be considered advantageous to the clinician in terms of ease of use and potential savings in chairside time and costs. This had led to the introduction of self-adhesive cements into the market in 2002. The bond to tooth structure is promoted by specific functional monomers, such as methacryloxyethyl trimellitate anhydride (4-META), 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) and dipentaerythritol pentaacrylate monophosphate (Penta-P), which differ among different commercial products. 14
According to the manufacturers, functional monomers are able to bond chemically to calcium hydroxyapatite, which helps in the retention of the restoration. A bond is formed between the hydroxyapatite of the smear layer, dentin or enamel with the acidic monomers, thereby creating a link between the ionized phosphoric acid and the network material.15 Self-adhesive cements were unable to demineralize/dissolve the smear layer completely, there is no decalcification/infiltration of dentin, and there is no hybrid layer and/or resin tag formation at the bonded interfaces. 16 ultilink N is a resin cement and is used with Multilink N Primer A & B. Multilink N Primer is a self-etching adhesive system, which is available in two bottles. One of the bottles contains the acidic monomers and the other contains the initiator solution. The phosphonic acid monomer which presents in the multilink N primer is responsible for it’s adhesive and self-etching effect.
Multilink Speed was developed to meet the demand among dentists for luting materials that offer easy, quick and universal application. There is no need for the application of conditioners or bonding agents to the dental hard tissues when Multilink Speed is used. Multilink Speed contains specifically formulated adhesive monomer that provides the cement with self-adhesive properties. This monomer consists of a long- chain methacrylate with a phosphoric acid group.
The mean values of microleakage of resin cements evaluated in this study were statistically significant at 2 months storage period at the cervical margin. The self-etch adhesive resin cements showed better performance `when compared to self-adhesive resin cements. Based on the results obtained in this study, the first null hypothesis must be rejected.
Ferracane et al., Stated that the acidity of the cement arising from the functional acid group of the monomer is controlled. It would be strong enough to promote hybridization with the tooth structure and low enough to prevent hydrophilicity, Which could compromise the marginal integrity of the material. Initially while making the mixture, the cement become hydrophilic that allows its flow and adaptation to the surface. Over time, as the acid group is consumed through the acid- base reaction with the minerals of dentin, the material becomes more hydrophobic. 17
But some studies, showed a limited capacity to demineralize and dissolve the smear layer in order to attain the adjacent dentin. The reason for the greater microleakage obtained with the self-adhesive cements are:
The high viscosity of the cement that makes it difficult for it to penetrate into the dentin tubules.
Lower penetration potential of acidic monomers of the self-adhesive cements into the smear layer that may interfere in hybrid layer formation. Thereby compromising the bond of self-adhesive cements.46
However, for the self-etching system Multilink N primer A/B, has the ability to form a very thin hybridized smear layer. The less micro leakage results obtained by the resin cement Multilink N are in agreement with other studies. One reason that may explain the less micro leakage results of the Multilink N is vigorous application of a self-etching primer, before luting with multilink N. Another reason is that the acidic monomer of self-etching system (Primer A + Primer B) is supplied in a separate bottle of water to prevent premature hydrolysis of the methacrylate. 18
The obtained results in this study are agreed with the findings of Ahmed Rabah, who evaluated the microleakage of indirect composite inlay cemented to with different cement strategies. They conclude that microleakage showed good results with self-etch luting resin cement strategy. 19
In the present study, in all samples of Multilink N group microleakage mean values were less compared to Multilink speed at both the storage periods on the occlusal surface. But they were not statistically significant.
This result indicates that using a self-adhesive cement to cement a composite inlay would offer comparable marginal integrity and durability to a self-etching resin cement.
Concerning the storage factor, statistical analysis revealed that the micro leakage mean values after 24hrs of storage and compared to mean values after 2 months were not statistically significant. But the mean ranks were less at 24 hours storage period than 2 months storage period for both supra gingival and sub gingival groups. The second null hypothesis was partially rejected.
These findings can be explained by the adhesive system degradation that probably occurs, as a result of hydrolysis that causes displacement of adhesive by water into the adhesive-dentin interface. Even though the degradation of naked collagen fibril by MMPs occurs into adhesive-dentin interface, In case of conventional resin cements with self-etching primer, due to their bond structure having less demineralized dentin the hydrolysis of adhesive resin may be more damaging to long- term bonding effectiveness. Additionally, the mechanical properties of the polymer network in the adhesive-dentin interface is altered by physical changes such as softening, plasticization, and chemical changes such as oxidation. The increased water sorption leads to a polymer plasticization, thereby reducing interchange interactions, such as entanglements and secondary bonds. Thus, this sponge effect results in reduction of the marginal integrity and polymer mechanical properties. For the two-step etch-and-rinse adhesive systems, the presence of water in their composition produces a semi-permeable membrane due it's high concentration of hydrophilic monomers and solvents. 20
Due to its complex pattern and lower mineral content, bonding to dentin is less predictable than enamel. Hence, Microleakage most commonly occurs when the gingival margin of any restoration is placed below the cementoenamel junction.9 In the present study, microleakage at cervical margin is high for multilink speed than multilink N for both supra gingival and sub gingival group. Because for supra gingival group the gingival margin was placed 1 mm above the CEJ and for sub gingival group the gingival margin placed 1mm below the CEJ.
Taschner et al. reported 29 of 62 restorations with 0.5 mm or less enamel left at the cervical margin. In their 2-year clinical study, these authors showed an acceptable performance of the self-adhesive resin cement. However, tooth integrity and marginal integrity were lower than for conventional multistep systems.Ansari ZJ, Motamedi MK compared occlusal and cervical microleakage of two self-adhesive cements and concluded that microleakage is greater in dentin margins (cervical) than in enamel (occlusal) margins. 9
In addition, thermocycling was reported as the main cause of increased microleakage. In the literature, dwell times are in between 4 and 30 seconds. Because dental tissues are poor thermal conductors, the dwell time was set at 30 seconds to compensate for the thermal inertia of the material and to allow thermal diffusion across the specimen.9 In the present study 500 cycles of thermal cycling at 50 c and 550 c was done according to the ISO TR 11450 – 1994.
Many studies have shown that for better bond strength between composite and resin cement, micromechanical retention of internal surface of indirect composites is also essential. It occurs due to loss of resin matrix and exposure of filler particles as a result of increasing effect of bond with resin. Different factors like pressure, particle size, type and hardness of particles, dimension of particles, tip size, distance from surface, angle of contact of particles with surface, time and speed of flow of particles should be considered in using air abrasion. 21
In the present study bonding surfaces of inlays were sandblasted using intra oral microetcher device, with 50 micron Al2O3 powder based on ortho technology for 5 min from 5mm distance and 60 PSI pressure.
The obtained results in the present study showed statistically significant difference between resin cements only at 2 months storage period for both supra gingival and sub gingival groups. But within the intra group or inter group comparison there was no statistically significant difference.
Although, the microleakage mean ranks were high for Multilink speed than Multilink N, found acceptable marginal integrity for Multilink speed. Clinical, longevity depends on the numerous steps before restoration is completed. Simplification is critical for a successful restorative procedure since many aspects need to be considered. A recent study evaluated the clinical performance of indirect restorations after using self-adhesive resin cement for 2years. The influence of selectively acid etching enamel prior to luting on marginal integrity, inlay integrity, tooth integrity, sensitivity, and complication of the restored teeth was assessed. The authors found acceptable clinical behavior in self-adhesive resin cement after two years of clinical service. Selective enamel etching prior to luting had no significant influence on marginal integrity, inlay integrity, tooth integrity, sensitivity, and complication of the restored teeth after 24 months.
Even though self-adhesive cements certainly represent an evolving technology in indirect restorative procedures, studies are necessary to evaluate the longevity of indirect restorations cemented with this category of resin cement over longer evaluation times.
Conclusion
Within the limitations of the present study, it can be concluded that
Within 24 hours storage period there is no much difference in micro leakage between Multilink N (self-etch primer adhesive resin cement) and Multilink speed (self-adhesive resin cement).
The greatest level of cervical microleakage was observed in Multilink speed (self-adhesive resin cement) than Multilink N (self-etch primer adhesive resin cement) after 2 months storage period.
In both the resin cements, there is little difference in microleakage levels after 2 months compared with 24 hours.