- Visibility 44 Views
- Downloads 7 Downloads
- DOI 10.18231/j.ijce.2020.033
-
CrossMark
- Citation
Management of internal inflammatory root resorption - an endodontic challenge: Case series
- Author Details:
-
Vasanta R Digole
-
Parag Dua *
-
Peeyush Pathak
-
Poonam Prakash
-
Vijay Kumar
Introduction
Root resorption is defined as a condition related to either a physiologic or pathological process leading to loss of hard tissues such as dentin, cementum or bone.[1] Andreassen has classified tooth resorption as internal and external root resorption. [2] The progressive destruction of intraradicular dentin and cementum occurs in internal root resorption resulting in a radiolucent area around the pulpal cavity. [3] The etiological factors for the internal root resorption includes traumatic injuries, infections and orthodontic tooth movement. [4]
Root resorption occurs in two stages, in first stage degradation of the inorganic mineral structure occurs followed by disintegration of the organic matrix. [5] Internal inflammatory resorption involves progressive loss of dentin and replacement resorption involves subsequent deposition of hard tissues like bone or cementum. [6] Clinically, the tooth with internal inflammatory resorption is usually asymptomatic which may be perforating or non-perforating resorptive defect. A reddish area pink spot, depicting the granulation tissue may show through the resorbed area. Internal resorption are often detected by visual examination based on colour changes in tooth crown, radiographic diagnosis, and cone beam computed tomography, microscopy. [7] Radiographic characteristic appearance reveal a round or oval radiolucent enlargement of the pulp space. The margins of the internal resorptive defect are smooth and well defined with distortion of the original outline of the canal space.
Various materials available for the treatment of internal root resorption include Mineral Trioxide Aggregate (MTA), Biodentine, glass ionomer cement, amalgam alloy, composite resin and thermoplastized gutta-percha administered either by injection or condensation techniques. Perforating internal resorption complicates the prognosis of endodontic treatment because of the weakening of remaining dental structure and possible periodontal involvement. To enhance the prognosis of the tooth MTA is most commonly used because of its biocompatibility, sealing ability and potential induction of osteogenesis. [8] This paper insights case series involving non-perforating and perforating internal resorption cases, which were successfully managed and showed successful healing after 6 months to 1 year follow-up period.
Case Reports
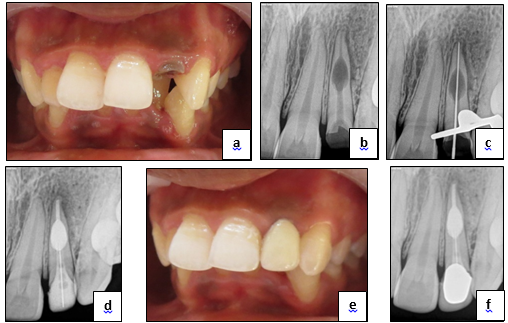
Case of non-perforating internal inflammatory root resorption
A 23-year-old female patient reported with a chief complaint of dull pain in upper right front tooth region since one month. She gave a history of trauma 9 years ago and refused to have any kind of dental treatment till reporting date. The clinical examination showed Eli’s class IV fracture and discoloured maxillary left lateral incisor, 22. Caries was also present with respect to tooth 22 [[Figure 1] a]. There was no associated swelling or sinus and the tooth mobility was within normal range. 22 was non-responsive on electric pulp testing. Radiographic examination revealed uniform oval radiolucency in middle third of root of the lateral incisor indicating a case of internal inflammatory root resorption, an associated radiolucency in the periapical area, and widening of periodontal ligament space and loss of lamina dura with respect to tooth No. 22 [[Figure 1]b]. The patient was informed about the prognosis of the tooth. A conservative orthograde treatment was planned for the patient which included filling of apical third of root canal and internal resorptive defect with MTA followed by post and core restoration with prefabricated fibre post and core build up with composite resin material.
Clinical procedures
After rubber dam (Hygenic, Colene Whaledent) application, access opening was initiated without local anaesthesia since the tooth was non-vital. The working length was established using electronic apex locator (Root ZX mini J Morita, Japan) and was confirmed on the radiograph with respect to tooth 22. During the instrumentation, 1% sodium hypochlorite and normal saline were used as irrigants. The irrigants were agitated with endoactivator (Dentsply, Tulsa Dental Specialities, Tulsa, USA) to enhance the removal of necrotic debris and microbial reduction from the inaccessible area of internal resorptive defect. After thorough biomechanical preparation, the prepared canal was dried with absorbent paper points, and an intracanal medicament of calcium hydroxide (ApexCal, Ivoclar vivadent) was filled completely within canal to achieve proper disinfection. Access cavity was sealed temporarily with Cavit-G (3M ESPE, Germany) and the patient was recalled after 1 week. Within a week the patient was asymptomatic. Obturation using bioactive material, MTA was planned. Hand plugger of corresponding size of apical diameter was selected. After drying the canal, MTA (MTA, Angelus) was manipulated and then incrementally placed into the canals and resorptive defect with MTA carrier. MTA was well condensed with hand pluggers. The canal was filled with MTA till the resorptive defect [[Figure 1]d], wet cotton pellet was placed, and closed dressing with cavit-G was given and recalled after 24 hrs. Next day, the setting and consistency of MTA plug was checked clinically with the help of probe. After confirmation of MTA setting, No.2 glass fibre post (Angelus, Brazil) was selected and luted with Dentsply Calibra dual cure resin cement (Dentsply clauk) and core build up was done with composite resin [[Figure 1]d]. After shade selection and tooth preparation for porcelain fused metal (PFM) crown, impressions were made and sent to dental laboratory for crown fabrication. At the final visit, the PFM crown was luted to the prepared tooth [[Figure 1]e]. The patient was recalled on a regular basis for upto 6 months [[Figure 1]f]. The follow-up radiograph after 6 month showed adequate peri-apical healing of tooth 22 and patient was clinically asymptomatic.
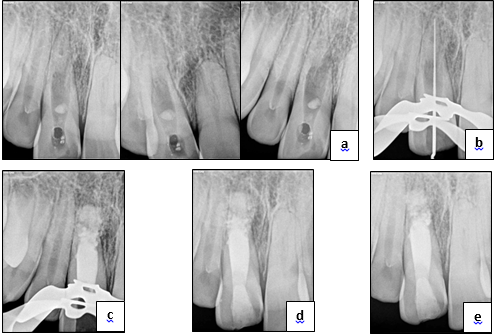
Case of perforating internal inflammatory root resorption
A 18 year old male patient reported with complaint of pain in upper front teeth region of jaw since 1 month. Medical history of the patient was non-contributory.[[Figure 2] a11 was non-responsive on electric pulp testing. Afterusing.[[Figure 2]b]Chemo-mechanicalirrigating solutionwas thenrecalled after 24[[Figure 2]c]. After the setting of the MTA plug the tooth was restored with composite resin material[[Figure 2]d].healing of the lesion [[Figure 2]e].
Discussion
There is always a dilemma of whether to treat a tooth with a questionable prognosis endodontically or extract it and subsequently plan for prosthesis e.g. dental implant. Bell first reported a case on internal resorption in 1830, since then there have been numerous reports in the literature. [9] Pathological root resorption leads to irreversible loss of tooth structure, and if the process is not stopped progression of resorption can may cause tooth loss. Diagnosis of root resorption depends on careful clinical and radiographic examination.
Internal root resorption is an inflammatory process initiated within the pulp space leading to loss of dentin and possible invasion of the cementum. [10] Treatment for internal resorption includes root canal therapy, followed by a definitive restoration. Presence of concavity defects and less dentin thickness in the internal resorptive lesions creates challenges for root canal instrumentation and filling procedures. Such lesion also acts as the reservoir of granulation tissues and clastic cells, which necessitates their complete elimination. [11] The chemical disinfection involves the use of different concentrations of sodium hypochlorite to disinfect the canal and dissolve the granulation tissue. Calcium hydroxide used as an intracanal medicament also helps to disinfect and dissolve any remaining granulation tissue. Both 1% sodium hypochlorite and calcium hydroxide were used in the present case series.
Root canal treatment will halt the resorptive process, but if the defect is too large, the tooth may mechanically fracture and fail. Like most disease processes, it is always best to identify these conditions early, and initiate proper treatment. Early diagnosis or detection of root resorption is important as it creates problematic situation for dental clinicians. If proper treatment protocol is followed while treating teeth with perforating defects, remineralisation of the resorptive defect and formation of hard tissue matrix may be observed. [12] In present case series MTA was used for remineralisation of the defect in case 1 and formation of the hard tissue barrier in case 2. In the present case series, different examples with conservative treatment approaches are included.
In case report 1, the endodontic management of the resorptive defect involved thorough chemo-mechanical preparation with gentle instrumentations to preserve the root dentin thickness. Irrigants were agitated with endoactivator for thorough removal of necrotic debris from resorptive defect. To achieve proper disinfection and cessation of osteoclastic activity calcium hydroxide intracanal medicament was placed within canal. To induce remineralisation and fill the internal resorptive defect bioactive material i.e. MTA was used. It was followed by Post and core restoration with prefabricated fibre post (Angelus, Brazil) luted with dual cure resin cement (Calibra Dentsply) and composite resin core built up. Later, PFM crown was luted to the prepared tooth to enhance the aesthetics.
In this case, during root canal shaping, the root canal was gently irrigated using 1% NaOCl. NaOCl is a widely used irrigation solution for the elimination of necrotic and granulation tissues from internal resorption cavities because of its enhanced antimicrobial activity and organic tissue dissolution capacity. [13] As a matter of precaution, a lower concentration of NaOCl solution was preferred to protect periradicular tissues from its toxic effects. [14], [15] In this case calcium hydroxide was used as an intracanal medicament as it maximizes the effect of disinfection procedures, helps to control bleeding, necrotizes the residual pulp tissue and dissolves any remaining granulation tissue. It also enhances the cessation of osteoclastic activity.
It was preferred to fill the root canal completely with MTA, because of its excellent biocompatibility, sealing ability, regenerative potential and single visit application. Also MTA is very well tolerated by the tissues. The tooth structure was thin and weakened in the resorptive defect, thus to reinforce and enhance the prognosis of the tooth a bioactive material, MTA was used. Because of the severe coronal tooth structure loss and large resorption cavity in the root canal a prefabricated fibre post16 was used in the present case to strengthen the root and facilitate the PFM crown fabrication.
In case report 2, extensive resorptive defect was seen with respect to maxillary right central incisor tooth No. 11. The similar approach was advocated for the management of this case also. MTA was indicated in because of the presence of a perforation of the root canal walls. It was used to fill the resorptive defect and formation hard tissue matrix because of its biocompatibility, sealing ability and potential induction of osteogenesis and cementogenesis.
Conclusion
For successful treatment outcome early diagnosis, removal of the cause, proper treatment of the resorptive defect of tooth is mandatory. The diagnosis of internal inflammatory root resorption is made through a combination of clinical and radiographic findings in daily practice. Considering the responsible mechanism behind the lesion, the treatment approach of such cases should be based on the immediate intervention once diagnosed, so that it may result in successful and prolonged outcome. Modern endodontic techniques including optical aids and ultrasonic improvement of chemical debridement should be used during the root canal treatment of internally resorbed teeth. Alternative materials such as calcium silicate cements like MTA offer new opportunities and better prognosis for the rehabilitation of resorbed teeth. Regular recall is important to check the status of healing and for the overall prognosis of the tooth.
Source of Funding
None.
Conflict of Interest
None.
References
- R F Ne, D E Witherspoon, J L Gutmann. Tooth resorption. Quintessence Int 1999. [Google Scholar]
- Leif Tronstad. Root resorption - etiology, terminology and clinical manifestations. Dent Traumatol 1988. [Google Scholar]
- S Patel, D Ricucci, C Durak, F Tay. Internal Root Resorption: A Review. J Endod 2010. [Google Scholar]
- F F Silveira, E Nunes, J A Soares, C L Ferreira, I Rotstein. Double ‘pink tooth’ associated with extensive internal root resorption after orthodontic treatment: a case report. Dent Traumatol 2009. [Google Scholar]
- S N Bhaskar. Orban's oral histology and embryology. 1986. [Google Scholar]
- M Fernandes, I de Ataide, R Wagle. Tooth resorption part I - pathogenesis and case series of internal resorption. J Conserv Dent 2013. [Google Scholar]
- S. Patel, A. Dawood, R. Wilson, K. Horner, F. Mannocci. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - anin vivoinvestigation. Int Endod J 2009. [Google Scholar]
- M Torabinejad, N Chivian. Clinical applications of mineral trioxide aggregate. J Endod 1999. [Google Scholar]
- T Bell. The anatomy, physiology, and disease of the teeth. 1830. [Google Scholar]
- . American association of Endodontics, “Glossary of endodontic terms. 2012. [Google Scholar]
- N Hedge, M N Hedge. Internal and external root resorption management: A report of two cases. Int J Clin Pediatr Dent 2013. [Google Scholar]
- N. Economides, O. Pantelidou, A. Kokkas, D. Tziafas. Short-term periradicular tissue response to mineral trioxide aggregate (MTA) as root-end filling material. Int Endod J 2003. [Google Scholar]
- M Haapasalo, Z Wang, Y Shen, A Curtis, P Patel, M Khakpour. Tissue Dissolution by a Novel Multisonic Ultracleaning System and Sodium Hypochlorite. J Endod 2014. [Google Scholar]
- M. E. Kaval, P. Güneri, M. K. Çalışkan. Regenerative endodontic treatment of perforated internal root resorption: a case report. Int Endod J 2018. [Google Scholar]
- M. Hulsmann, W. Hahn. Complications during root canal irrigation - literature review and case reports. Int Endod J 2000. [Google Scholar]
