- Visibility 78 Views
- Downloads 6 Downloads
- DOI 10.18231/j.ijce.2021.026
-
CrossMark
- Citation
Palato-gingival groove: A silent nidus. Recognition and an innovative management approach: A report of 3 cases
- Author Details:
-
Purushothama Rangaswamy *
-
Sri Harsha Tummala
-
Samrat R Magarvalli
-
Sujith Ramachandra
-
Kavitha Govindappa
-
Shwetha E
Introduction
Palatogingival groove is a rare developmental anomaly usually found on the palatal aspect of maxillary anterior teeth.[1] Region of maxillary anterior teeth are considered to be an area of embryologically importance with major and minor malformations [such as Palato-gingival groove (PGG), Dens-in-dente]. The region in which the lateral incisors are located are considered to be an area of embryologically risk.[2] The incidence of radicular grooves is reported to be between 2.8 to 18%, among which the most prevalent are the Maxillary Lateral Incisors.[3] Palato-gingival Groove has different synonyms such as; Palato-radicular Groove, Disto-lingual Groove, Radicular Lingual Groove, Corono-radicular Groove, Cingulo-radicular Groove, Vertical developmental Radicular Groove and Interruption Groove.[4]
Maintenance of proper oral hygiene is questionable due to the presence of defective grooves. Resulting these areas act as a hidden trap in the tooth [as a nidus] for plaque accumulation which destroys the sulcular epithelium and later deeper parts of the periodontium, resulting in periodontal destruction with or without pulpal pathologic change.[5] Finally, if is left untreated over a period of time, it can lead to serious localized periodontal lesion or can communicate with endodontic lesion.
Route cause for PGG was first explained by Black in 1908, as a radicular groove.[6] In 1958, Oehlers first reported radicular invagination of a maxillary lateral incisor.[7] It has a similarity to dens invaginatus; however, it differs from it in such a way that it occurs due to an unfolding of the epithelium (resulting in a groove), rather than an invagination (resulting in a circular opening).[8] Some researchers have also claimed that the anomaly might results from an attempt to form another root. [9] Some authors proposed that this defect is a mild form of dens invaginatus.[10]
Extension of grooves by different studies have shown that in lateral incisors.[11]
|
43% |
The grooves shows less than 5mm into the root extension. |
|
47% |
Between 6-10mm |
|
10% |
Shows more than 10mm |

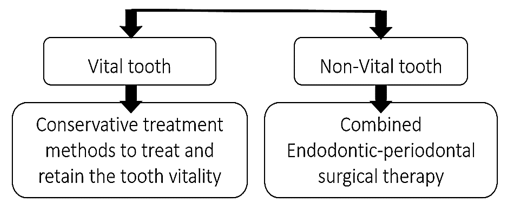
Treatment of PGG
Basic principle for treatment plan
Complete elimination of microbial colony,
Morphological alteration and sealing of the defective groove,
Periodontal therapy: Periodontal regeneration [attachment] and complete healing of the periodontium.
First, it is necessary to examine whether the pulp is involved in the pathologic change;
Case Report – 1
A 55-year-old female patient reported to the department of Conservative Dentistry and Endodontics, Sharavathi dental college and hospital, Shivamogga, Karnataka, with the chief complaint of decayed teeth in upper front teeth region. On clinical examination class-III dental caries with respect to maxillary right lateral incisor, on careful examination on the cingulum there was a small groove, and clinically small reflection of sulcular gingiva was reflected and a methylene dye penetration test was carried out to know the extension of the defective groove. On radiographic evaluation, a small radio-opaque line in the mid portion of the crown less than 3mm was noted.
The case was diagnosed as reversible pulpitis with PGG (grade-0).
After proper isolation, caries excavation and groove saucerization was done by using round and long tapered diamond burs. Finally, the tooth was restored with composite resin. Post-operative guidelines were explained to the patient as regular oral mouth rinse and proper brushing habits. Regular re-checkup was advised for every 2 months.
![Restorative Management of PGG irt 12 [Case - 1]](https://s3-us-west-2.amazonaws.com/typeset-prod-media-server/93886881-55dc-4d80-940b-d4ab8cf16347image3.png)
Case Report – 2
A 28 years old female patient came to the department of Conservative Dentistry and Endodontics, Sharavathi dental college and hospital, Shivamogga, Karnataka, with the chief complaint of discolored tooth and occasional discharge of pus from left upper front tooth region from 6 months. Past history reveals non traumatic condition. General medical history was noncontributory. On clinical examination, a discolored Maxillary Left Central Incisor was found but neither tooth mobility nor any swelling was detected. On palpation there was no bony depression found. A pit along with a groove was found on the palatal aspect of Maxillary Left Lateral Incisor tooth near the cingulum. On clinical probing, attachment loss extension on to the root surface and pocket was approximately 6mm in depth. Pulp vital examinations were carried out. Radiographic evaluation revealed periapical radiolucency of about 3mm above the Maxillary Left Central Incisor with mature apex. An anomalous internal structure consists of a straight radio-opaque line running from the cingulum area to cemento-enamel junction. The anomaly was detected as palatogingival groove in Maxillary Left Lateral Incisor.
The case was diagnosed as apical periodontal abscess for Maxillary Left Central Incisor and palato-gingival groove PGG = (grade-1) in Maxillary Left Lateral Incisor.
Extensive treatment options were discussed with the patient. Preprocedural treatment protocol like complete oral mouth rinse with 1.5% CHX oral rinse. After complete oral prophylaxis, proper isolation protocols were followed and multiple visit non-surgical endodontic treatment protocol was performed for Maxillary Left Central Incisor, under Local anesthesia.
Periodontal therapy: Periodontal flap surgery was planned under local anesthesia. A crevicular incision was given in respect to 21 and the full-thickness flap was raised. After flap reflection defective groove was clearly traced by using methylene blue dye, curetted and cleaned and after this, the groove was corrected (saucerization) with a long thin tapered diamond bur and finally walls were smoothened with composite finishing bur. After achieving proper isolation, the defective groove was filled with Bio-dentin material and finally self-cured resin cement for final coronal restoration was done for 21. Post-operative instructions were advised to rinse her mouth with chlorhexidine mouth rinse (0.2%) twice a day for 2 weeks. Recall examination reveals normal healing and asymptomatic conditions.
![Minor Surgical Management of PGG irt 22 [Case - 2]](https://s3-us-west-2.amazonaws.com/typeset-prod-media-server/93886881-55dc-4d80-940b-d4ab8cf16347image4.png)
Case Report – 3
A 35-year-old female patient reported to the department of Conservative Dentistry and Endodontics, Sharavathi dental college and hospital, Shivamogga, Karnataka, with the chief complaint of pus exudation and persistent dull pain in upper left front teeth region from the last 4 months. Patient reveals history of trauma 5 months back (self-fall from stairs). Past Dental history reveals root canal treatment was initiated for Maxillary Left Central Incisor 4 months back and undergone extraction of Maxillary Left Lateral Incisor due to poor periodontal condition.
On clinical examination, discolored tooth and there was pus exudation from the gingival sulcus of the palatal aspect of Maxillary Left Central Incisor. The affected tooth was tender to percussion. On careful periodontal probing, a deep groove extending from the cingulum to the mid root area was noted. Radiographic examination with a radio-opaque material placed into the groove gave the exact length, apical location and termination of the Palato-radicular groove. Further radiographic examination revealed extensive alveolar bone loss in relation to Maxillary Left Canine. To eliminate the radicular groove and promote periodontal regeneration, endo - periodontal surgical treatment was planned.
The case was diagnosed as chronic apical periodontal abscess for Maxillary Left Central Incisor with palato-gingival groove. (grade-2).
After the oral prophylaxis, multiple visit non-surgical endodontic treatment (re-rct) was performed for Maxillary Left Central Incisor. The area was anesthetized and mucoperiosteal flaps on both labial and palatal aspects were elevated. Thorough degranulation of the lesion was performed. An advanced circumferential bony defect was found after degranulation. The palatal radicular groove was eliminated by means of saucerization using a long-tapered diamond bur. After the saucerization groove was sealed with Biodentine.
Alloplastic bone graft and GTR membrane placement
The flap was readapted, placement of alloplastic bone graft and to prevent the graft material from getting displaced, Hydroxyapatite graft material was mixed with saline and placed into the deep bony defect. It was followed by placement of GTR membrane (Heli guide) to promote periodontal regeneration and to avoid formation of long junctional epithelium. After flap closure with suture materials, the surgical area was covered with a non-eugenol periodontal dressing (Coe Pak). The patient was prescribed antibiotics and non-steroidal drugs for a week. The patient was asked to rinse her mouth with chlorhexidine mouth rinse (0.2%) twice a day for a week for chemical plaque control measure.
At 1-week post-surgery follow-up, the periodontal pack and sutures were removed. The patient was recalled at regular intervals of 3, 6, 9, 12 months for follow-up. After 3 months, the clinical probing depth had reduced from 8 to 3 mm and the area was periodontally healthy.
![Case-3: Endo-Perio Surgical Management of PGG irt 21 [Case - 3]](https://s3-us-west-2.amazonaws.com/typeset-prod-media-server/93886881-55dc-4d80-940b-d4ab8cf16347image5.png)
Discussion
Palato-radicular grooves [PRG] are a unique deformity in the process of tooth development. PGG acts as a podium for bacterial growth, leading to complicate the prognosis for the affected tooth to survive. Generally, PGG is reported with dull intermittent [12], [13] or acute pain, [14], [15] mobility of the teeth, [16], [17] pain on percussion, [12] pus discharge, [18], [19] sinus tract formation [20], [17] and gingival swelling. [14] It can also be found in asymptomatic conditions. [17] Among the three case reports presented, case-report-1 patient had history of dental caries, case-report-2 patient did not report any signs and symptoms, whereas in case-report-3 patient gives history of trauma, discoloration of the teeth and with grade-I mobility. Pulp vitality was retained or lost based upon pulpal nerve involvement. Here in case (case-report – 1 and 2) = pulp vitality was positive, where as in case-report-3 = negative pulp vitality was observed.
The diagnosis of PGG is depended on signs and symptoms of the lesion. Careful clinical examination of anatomical sites and investigations such as tooth vitality tests, clinically by trans-gingival probing to detect the defective groove, and radiographic examinations. Unlike symptomatic condition (case-report 3), PGG can be diagnosed early at asymptomatic stage (case-report 1 and 2) thus preventing damage to the tooth and periodontium.
The location of the groove, depth, and length of the groove (shallow/deep) or (long/short) and the extent and accessibility of the periodontal defect, eventually decides the prognosis of teeth. The rationale behind the selected treatment plan was the following: Prevention of the plaque accumulation by saucerization of the groove, to seal the defective area with biocompatible restorative materials, to allow the re-adaptation and approximation of the flap to the root surface to prolong the survival of the tooth.
Teeth associated with simple groove and no periodontal destruction can be treated by superficial odontoplasty and curettage of the granulation tissue as a periodontal therapy. [21], [22] However, for complex PGG surgical intervention along with patient education for maintaining oral hygiene is must. If groove extension is deep or up to the apical third then surgical intentional reimplantation therapy [23] may be one of the option or surgical extraction is recommended.
Dragoo et al explained the criteria for the subgingival restorative materials for sealing of this type of lesion should have ideal required properties as biocompatible to the tissues. [24] Many biocompatible materials like starting from amalgam, GIC, bio-ceramic materials, silicate cements, etc. Among those Biodentine, a tricalcium silicate-based material popularly known as “dentin replacement and repair material”. It has proven bioactive properties, is known to promote hard tissue regeneration and is biocompatible. The ability to form hydroxyapatite crystals at the surface especially when formed at the dentin material interface is known to improve its sealing ability. [25] Based on their properties, Biodentine material is chosen in the case-report-3 as a subgingival filling material for the defective PGG. Whereas superficial defective grooves (in case report-1) were restored with bio-ceramic dual cure composite resins. And a combination (as in case report-2) of both Biodentine was used for subgingival PGG defect and composite resin for PGG defect above the gingival level.
Various regenerative materials such as bone graft, platelet-rich plasma [PRP], plasma-rich fibrin [PRF] have been used based on the size of the defects. Since decade guided tissue regeneration (GTR) has been used as a regenerative material which prevents the epithelial downwards growth and allows the growth of periodontium, cementum, and bone. McClain et al. proclaimed that combined usage of graft/GTR promotes certain attachment levels. [26] In the case-report–3, with the combined technique we were able to achieve significantly better results at the 6 months follow-up than open flap debridement alone. Anderegg and Metzler have reported clinical success of about 62% of cases at the 6 months follow-up for cases treated with resorbable barriers. The combined technique used among those 10% of the cases were able to reduce pocket depth by 8.0 mm, a significantly better range than the cases that are treated by open flap debridement. [27] McLain and Schallhorn also showed that attachment levels are maintained more predictably in sites treated with a combined graft/GTR therapy. The results achieved in this patient are comparable to those reported for bone allograft/expanded polytetrafluoroethylene therapy in intra-bony defects without the need for a second procedure for membrane removal. [25], [28]
With the new options in diagnosis and treatment, clinicians need a detailed understanding of the characteristics, treatment, and prognosis of PGG to successfully manage the condition in order to ensure the survival of the tooth.
Conclusion
Diagnosis and treatment of palatogingival groove is often dilemmatic in clinical conditions. Early identification of this anomaly is highly recommended to prevent the loss of vitality of the tooth. Presence of a palatogingival groove does not always imply that pathology will develop. Depending on the extension of the defect on the root surface there may be a breach in the epithelial attachment subsequent to post plaque-retention resulting in progressively advancing inflammation. The groove may undetected and it has always been a dilemma while diagnosing. Thorough clinical examination of the lingual surface of incisors should be encouraged as a part of the routine protocol. However clinical macroscopic analysis of the groove does not allow precise evaluation of the extent and degree of the defect, so in combination of microscopic analysis by using various aids in magnification (loops, dental operating microscopes) plays a major role in definitive diagnosis in future era. A proper diagnostic procedure and an adequate treatment planning are necessary for preventing the localized condition. PGG defect treatment involves multidisciplinary approach and the concerned tooth must be maintained and kept under constant re-evaluation.
Conflict of Interest
The authors declare that there are no conflicts of interest in this paper.
Source of Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- SK Dana, GD Khan, JA Joy, MS Khatib. An Innovative Management of Palato Gingival Groove In A Maxillary Lateral Incisor. Univ J Dent Sci 2020. [Google Scholar] [Crossref]
- A Dharamsi, L Garhnayak, M Garhnayak, G P Singh, V Chaturvedy. Comprehensive management of a lateral incisor with a deep palate-radicular groove: a case report. Indian J Stomatol 2011. [Google Scholar]
- G L Hou, C C Tsai. Relationship between palato-radicular grooves and localized periodontitis. J Clin Periodontol 1993. [Google Scholar]
- JA Withers, MA Brunsvold, WJ Killoy, AJ Rahe. The Relationship of Palato-Gingival Grooves to Localized Periodontal Disease. J Periodontol 1981. [Google Scholar] [Crossref]
- CG Devaraj, A Yadav, R Kapoor, P Mishra, S Godara, M Meena. Palatoradicular Groove Associated Defect Resolved with GIC, Alloplastic Graft and GTR Membrane. J Mahatma Gandhi Univ Med Sci Tech 2016. [Google Scholar] [Crossref]
- G V Black. Operative dentistry: pathology of the hard tissues of teeth. 1908. [Google Scholar]
- FA Oehlers. The radicular variety of dens invaginatus. Oral Surg, Oral Med, Oral Pathol 1958. [Google Scholar] [Crossref]
- TG Gound, GI Maze. Treatment options for the radicular lingual groove: a review & discussion. Pract Periodontol Aesthet Dent 1988. [Google Scholar]
- Marshall D. Peikoff, John B. Perry, Lorne A. Chapnick. Endodontic failure attributable to a complex radicular lingual groove. J Endod 1985. [Google Scholar] [Crossref]
- K W Lee, E C Lee, K Y Poon. Palato-gingival grooves in maxillary incisors. A possible predisposing factor to localized periodontal disease. Br Dent J 1968. [Google Scholar]
- D Rachana, P Nadig, G Nadig. The palatal groove: Application of computed tomography in its detection - a case report. J Conserv Dent 2007. [Google Scholar] [Crossref]
- V Arora, SR Srinivas, P Arora, KD Jithendra, S Shetty. Surgical management of a palatal radicular groove and an associated periodontal lesion in a maxillary lateral incisor. J Pierre Fauchard Acad (India Section) 2009. [Google Scholar] [Crossref]
- AG Bharwani, D Mundinamane, A Suchetha, R Heralgi. Treatment of an intrabony osseous lesion associated with a palatoradicular groove. Contemp Clin Dent 2012. [Google Scholar] [Crossref]
- S Sharma, P Deepak, S Vivek, RS Dutta. Palatogingival groove: recognizing and managing the hidden tract in a maxillary incisor: a case report. J Int Oral Health 2015. [Google Scholar]
- J Forero-López, L Gamboa-Martínez, L Pico-Porras, JL Niño-Barrera. Surgical management with intentional replantation on a tooth with palato-radicular groove. Restor Dent Endod 2015. [Google Scholar] [Crossref]
- NV Ballal, V Jothi, KS Bhat, KM Bhat. Salvaging a tooth with a deep palatogingival groove: an endo-perio treatment – a case report. Int Endod J 2007. [Google Scholar] [Crossref]
- M Rajendran, K Sivasankar. Palato-radicular groove hidden route to destruction-case report. Int J Curr Res Rev 2013. [Google Scholar]
- A Gandhi, P Yadav, T Gandhi. Endodontic-periodontal management of a maxillary lateral incisor with an associated radicular lingual groove and severe periapical osseous destruction-a case report. J. Ir Dent Assoc 2012. [Google Scholar]
- K Al-Hezaimi, J Naghshbandi, J H Simon, I Rotstein. Successful treatment of a radicular groove by intentional replantation and Emdogain therapy: four years follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009. [Google Scholar]
- P Castelo-Baz, I Ramos-Barbosa, B Martín-Biedma, AB Dablanca-Blanco, P Varela-Patiño, J Blanco-Carrión. Combined Endodontic-Periodontal Treatment of a Palatogingival Groove. J Endod 2015. [Google Scholar] [Crossref]
- S F Robison, R L Cooley. Palatogingival groove lesions: recognition and treatment. Gen Dent 1988. [Google Scholar]
- JH Jeng, HK Lu, LT Hou. Treatment of an Osseous Lesion Associated With a Severe Palato-Radicular Groove: A Case Report. J Periodontol 1992. [Google Scholar] [Crossref]
- H Yan, N Xu, H Wang, Q Yu. Intentional Replantation with a 2-segment Restoration Method to Treat Severe Palatogingival Grooves in the Maxillary Lateral Incisor: A Report of 3 Cases. J Endod 2019. [Google Scholar]
- Dr, Dr Manoj Priyanka Madale, Dr Likhitkar. Ashwini Kelode, Dr. Milind Ambhore and Dr. Vivek Tattu anomaly in maxillary anterior region”. International Journal of Current Research . [Google Scholar]
- DA Johns, VY Shivashankar, K Shobha, M Johns. An innovative approach in the management of palatogingival groove using BiodentineTMand platelet-rich fibrin membrane. J Conserv Dent 2014. [Google Scholar] [Crossref]
- P K Mcclain, R G Schallhorn. Long-term assessment of combined osseous composite grafting, root conditioning, and guided tissue regeneration. Int J Periodontics Restor Dent 1993. [Google Scholar]
- CR Anderegg, DG Metzler. Treatment of the Palato-Gingival Groove With Guided Tissue Regeneration. Report of 10 Cases. J Periodontol 1993. [Google Scholar] [Crossref]
- S Oreamuno, V Lekovic, EB Kenney, FA Carranza, HH Takei, B Prokic. Comparative Clinical Study of Porous Hydroxyapatite and Decalcified Freeze-Dried Bone in Human Periodontal Defects. J Periodontol 1990. [Google Scholar] [Crossref]
