Introduction
The dental pulp is a sterile connective tissue protected by enamel, dentin, and cementum. Significant injury of the pulp chamber leads to inflammation and may result in pulp necrosis if left untreated. Possible scenarios that can result in periapical radiolucencies are commonly initiated either by trauma, caries, or tooth wear.1 Pulp disease and bacterial infection of the pulp space, result in periapical lesions.2 These lesions are mainly revealed during routine radiographic examinations or an episode of extreme pain reported by the patient.3 Periapical lesions are classified as radicular cysts, dental granulomas or abscesses.4, 5
Among these lesions, those that are larger in size are usually radicular cysts. Some of these large lesions, however, may appear to be granulomas. 2 The main purpose of all endodontic treatment, specially cleaning and shaping, is to remove necrotic tissue and eliminate infective bacteria. 6 Root canals are usually not properly prepared in apical third and thorough disinfection of this zone cannot be expected; therefore, complete obturation of the prepared, cleaned and shaped canal space is necessary. 7 Proper obturation lowers the chances of coronal leakage and bacterial multiplication. It also seals the apex from periapical tissue fluids and the remaining irritants are buried within the canal.2 Pulp exposures as a result of trauma, can lead to pulp necrosis and periradicular pathosis as it can be colonized after losing it blood supply. 8 Microorganisms and their products have a crucial role in the initiation, progression, and establishment of periradicular conditions. 1 Exposed carious pulp, invaded with microorganisms, is an area of progressing of inflammation and result in pulp necrosis. Once root canal is infected, and pulp necrosis is established, local blood supply is absent, therefore, neither host defense nor systemic antibiotic therapy would be effective in restricting the infection. 9 Here comes the role of non-surgical endodontic treatment preventing successfully their spread. It has been reported that the fluids within root canal(s) contains a suspension of endodontic bacteria. The root canal walls, however, hold biofilms and bacterial aggregates forming concentrated bacterial centers. 10 Dentinal tubules and root canal complexities are the seat of infections. These infections can be treated using endodontic procedures or extraction. The goal in endodontic treatments is preserving a healthy functional tooth without a surgical treatment. 2 Conservative nonsurgical techniques should be the considered treatment of all inflammatory periapical (e.g. orthograde root canal therapy). Only after failing of nonsurgical procedures, surgical intervention is suggested. Moreover, surgery has limited use in the treatment of periapical lesions due to its many disadvantages. Treating teeth with periapical lesions following an endodontic procedure, has been reported to have a success rate of 85%. Both complete and partial healing of periapical lesions after nonsurgical endodontic therapy has an incidence of 94.4%. 2
Case Report
A 25-year-old female in a good general health presented to the Department of conservative dentistry and endodontics at the dental clinic of Monastir with the chief complaint of persistent mild pain in the right maxillary anterior tooth region. The patient reported a history of trauma to her anterior teeth when child. The intraoral examination revealed that teeth 11 was tender on percussion. Vitality testing was negative for the tooth suggesting pulp necrosis. Normal gingiva health was confirmed on periodontal probing.
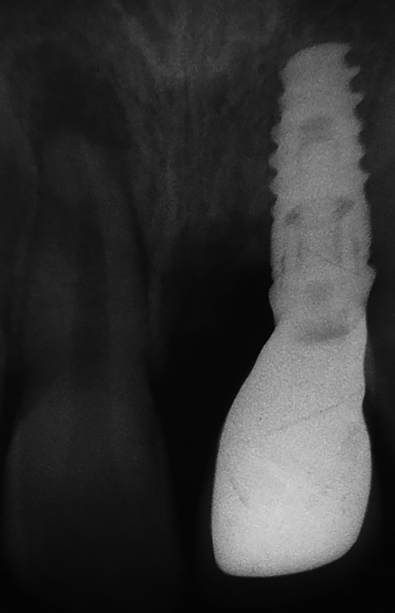
However, intraoral periapical radiograph revealed moderate size periapical lesion with will-defined borders involving the apices of teeth 11 (Figure 2). The clinical diagnosis was chronic periapical periodontitis.
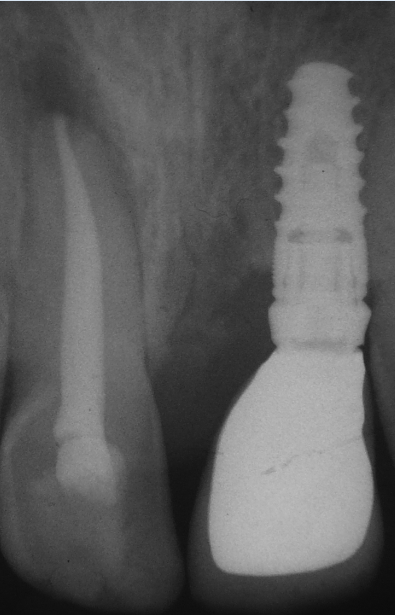
Non- surgical endodontic therapy was planned. Under rubber dam, the access cavity was prepared and root canals were shaped and cleaned using instrumentation nickel titanium instruments (2 shape, Micro Mega). The canal was then thoroughly irrigated with 2.5% sodium hypochlorite at each instrument change. Root canal length was estimated with an electronic apex locator (Rootor, META BIOMED) and the length was confirmed by further radiograph (Figure 3). After biomechanical preparation of canals to an apical size of 30, calcium hydroxide paste (Ultracal, Ultradent Products, Inc., South Jordan, UT, USA) was dispensed into the canal as intracanal medicament and access cavities was sealed with temporary filling (MD-TempTM, META Biomed co).
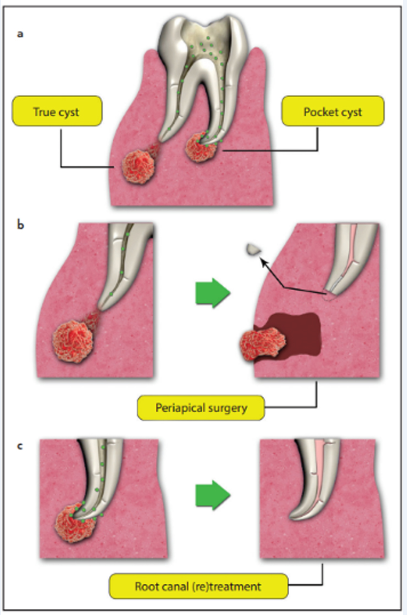
Figure 1
Infection in the root canal space causes periapical cysts categorized as true or pocket cysts; (a): The true cysts are resolved after periradicular surgery; (b): while root canal (re)treatment can resolve most of the pocket cysts without surgical intervention (c). 2
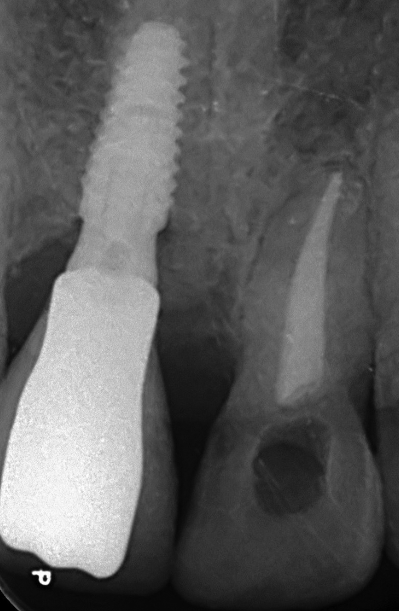
Three weeks later, patient’s second visit reveals an asymptomatic tooth. Coronal temporary filling was removed after application of dental rubber dam. 5.25% sodium hypochlorite was used to remove intracanal calcium hydroxide and root canal irrigation. The root canal was obtured with bioceramic sealer (BioRoot RCS, Septodont) and gutta-percha points via cold lateral compaction technique ($). The access cavity was filled with composite resin Filtek Z350 XT (3M ESPE, St. Paul, MN, USA).
After 2 years of follow-up, the patient was asymptomatic and periapical radiograph revealed a high resolution of the lesion with significant bone formation (Figure 5).
Discussion
Pulp necrosis commonly occurs due to trauma or dental caries, which makes root canal system, highly exposed to microorganisms’ colonization. 11 These microorganisms along with other cell components residing in the root canal may generate an inflammatory process in periapical tissues and contributes to the initiation and establishment of periradicular lesions. 12, 13 It is a barrier that prevents the spread of microorganisms into the surrounding tissues and result of a localized inflammatory response to infection. 14 The bone is resorbed then substituted by a granulomatous tissue and polymorophonuclear leukocytes' dense wall (PMN) which is identified as radiolucency on radiographic images. 13 Some microbial products and toxins can initiate and establish the periradicualr pathosis after crossing this barrier. 13 The host reacts to this invasion of microbes, which causes the development of different lesions with various histological and clinical images such as: acute and chronic periapical inflammations, chronic suppurative periapical inflammation, acute periapical abscess/cellulitis, granulomas and cysts. 15 Non-surgical root treatment should be considered as the standard therapeutic option for teeth with periapical radiolucencies regardless of the histological diagnosis and thus reducing to the minimum possible the load of microorganisms in the root canal systems. 16 Root canal treatment of teeth with periapical lesions healing process and a highly successful procedure with a survival rate of 95% after a 4-year follow-up. 17 Surgical intervention should be considered only after failing of nonsurgical root canal treatment. 18 Failure of endodontic treatment may be associated with persistent intraradicular infection, in uninstrumented root canals and dentinal tubules plus the irregularities of the root canal system. 13 In order to achieve the above purpose, shaping and cleaning of the root canals aided with calcium hydroxide as intracanal medicament is recommended. Root canal treatment aims to eradicate or significantly reduce and control the bacterial invasion to ensure periradicular tissue healing of the apical periodontitis, it can be achieved only if chemical irrigation sustains mechanical instrumentation. In fact, the irrigant will induce debris flushing, dentinal walls lubrication, organic components dissolution, and will lessen bacterial load in the root canal. In several studies, 1–5% sodium hypochlorite (NaOCl) solutions are reported to have an important spectrum antimicrobial activity. 19 An increase in NaOCl solution concentration is associated with an increase in the antibacterial activity. 20
Antimicrobial property is always improved by copiously irrigating using larger volumes. In the present case report, calcium hydroxide was used as the intracanal medicament for two weeks. Calcium hydroxide is widely used as an intracanal medicament for teeth with periapical lesions, because of its various biological properties. The dissociation of calcium hydroxide into calcium and hydroxyl ion in aqueous solution is responsible for its antimicrobial activity. Also, it provides a high alkaline environment with pH value of 12, where most of the microorganisms are unable to survive. 18 It has actions like anti-inflammatory, neutralizing acid, inducing cell differentiation and neutralizing exotoxins. All these actions ultimately lead to the periapical healing.
After chemical-mechanical debridement and removal of microorganisms, all canals must be sealed hermetically to eliminate and to prevent microorganisms recolonizing the root canal system. 15
Thus, root canal obturation involves the 3D filling of the entire root canal system and must eliminates all avenues of leakage from the oral cavity or the periradicular tissues into the root canal system. Bioceramic-based sealers have overpowered other sealers because of their biocompatibility chemical stability, flowability, hydrophilicity, biomineralization, calcium ion release, and hydroxyapatite formation. Thus, these qualities ameliorate the hermiticity of root canal obturation and consequently promote the healing of periapical lesions as well. 21
In our clinical case, we used BioRoot™ RCS which creates an alkaline environnement by raising the pH wich could be caused by the Ca2+ and OH− leaching preventing bacterial proliferation and stimulates periodontal and endodontic tissue regeneration. This sealer is interesting option for the use of the single-cone technique; their physical proprieties render them capable of providing a stable three-dimensional seal in the necessary time fram, all without the need for warm compaction procedures. A small amount of cement was placed into the canal bringing it up to the proper length. After, a gutta-percha cone is inserted to constitute the central part of the obturation. Thus, this single cone hydraulic condensation technique is simple and fast. The gutta percha point is used as a plunger to push the sealer into the fine parts of the canal and in cases of retreatment to act as a path tooth apical foramen. 22
In our case, the radiograph showed bone thickening and complete resolution of the periapical radiolucency. These result can be attributed with the properties of BioRoot™ RCS. It possess a great adhesion to dentin and gutta percha and form chemical bond with dentin as it forms hydroxyapatite in the presence of moisture because of it hydrophilic nature. Therefore, it affords hermetic obturation of the apical foramen, isthmus, and accessory canals. Camps et al. suggested that the BioRoot has the potential to induce angiogenesis and osteogenesis which are essential for periapical tissue regeneration. 23
Conclusion
The non-surgical endodontic treatment described in this article demonstrated an excellent healing of periapical lesions through proper debridement, disinfection and three dimensional obturation of the root canal system. The calcium hydroxide can helps in periapical lesion’s healing effectively. This minimally invasive procedures offer a high rates of healing for this lesions.