Introduction
Non-restored nonvital teeth are structurally compromised and represent one of the greatest challenges for the clinician. More than 15 years ago, the restoration of endodontically treated teeth was automatically associated with a combination of prefabricated or custom made metallic post and cores and full crowns.
Various post materials and designs have been introduced over the years; a considerable amount of sound coronal and radicular tooth structure was sacrificed, increasing risk of root perforation or fracture. However, recent motivation to protect and reinforce the remaining sound tooth structure, bolstered by the properties of modern adhesive systems, has encouraged clinicians to re-evaluate the dogma of traditional restorative dentistry. Looking for alternative methods to build up nonvital teeth has become increasingly popular. Adhesive restorations allow clinicians to create minimally invasive preparations, thus preserving sound tooth structure; interestingly, the continuous improvement of the physical and mechanical properties of resin bonded composite (RBC) has encouraged clinicians to progressively abandon amalgam.1
Fibre-reinforced composites advocated for use as post-and-core systems can be classified into two categories: prefabricated posts and customized posts. When the post’s section differs from that of the canal, the luting technique creates a thick layer of cement between the root dentin and the post and this interface becomes the weakest point. Customized fibre post– core systems were produced to overcome this problem.2 An example for the customized fibre post–core system is Ribbond (Ribbond Inc., Seattle, WAUSA), which is commercially available and was first introduced as a splint material. The material has a three-dimensional structure due to the leno weave or triaxial braid, and this provides mechanical interlocking with composite resin at different planes. In addition, microcracking is minimized during polymerization of the resin.2
Case 1
A 65 year old patient reported with a chief complaint of broken teeth in lower right back tooth region. Patient gave dental history of root canal treatment in the same tooth 5 years back. Patient had no pain. On clinical examination, there was root stump w.r.t. 45. On radiographic examination, periodontal ligament widening was seen. On the basis of clinical and radiographic findings, a diagnosis of apical periodontitis was made w.r.t. 45. Retreatment followed by buildup with ribbond fibers was planned. A written consent was taken from the patient after explaining the treatment protocol. In the first visit, retreatment was done. The old guttapercha was removed using H files and was checked radiographically. The working length was determined using #15 K-file and confirmed radiographically. Biomechanical preparation was done by K files using step back technique. Irrigation was done using 5.25% NaOCl and saline). Chlorhexidine was used as a final irrigant. Mastercone was selected according to the last apical file used. The canals were dried with paper points and obturated by lateral condensation technique. Sealer used was Roeko, Germany. In the second visit, the post endodontic restoration was done using Ribbond Fibers. The GP was sheared till 4-5 mm below the CEJ. Ribbond fibers were dipped in the bonding agent. After etching and conditioning, the ribbond fibers were packed in the canal along with flowable and packable composite.
C ase 2
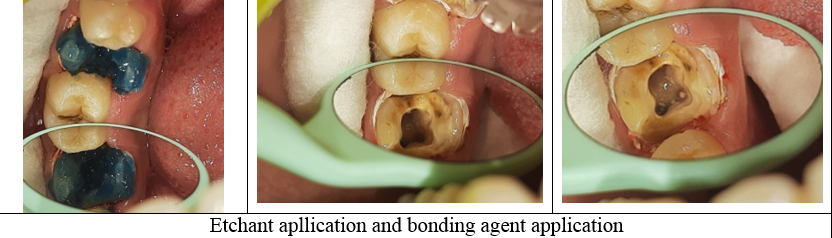
A 22 year old female patient came with a chief complaint of pain on chewing food in upper right back tooth region of mouth since 2 weeks. On clinical examination grossly decayed maxillary first molar was observed. Tenderness on vertical percussion was present i.r.t 16. The treatment plan advised was non-surgical root canal treatement i.r.t. 16. On radiographic examination periapical lesion was associated i.r.t. 16. The working length was confirmed radiographically using #15 K-file. Coronal flaring was done using Sx (Protaper Gold File System. The remaining root canal system was prepared with rotary file system using Protaper Gold File System till F2 with copious irrigation using 5.25% sodium hypochloride solution. Mastercone selection was done using 25.06 guttapercha. The canals were dried with paper points and obturated by laterally condensed guttapercha (Roeko, Germany) root canal sealer. The treatment was completed in 2 visits. The post endodontic restoration was done using RibbondFibers, after etching and conditioning of the prepared cavity the fibers were cut wetted with bonding agent and placed inside the isolated cavity along with flowable and packable composite.
Case 3
An 18 year old male patient came with a chief complaint of continuous pain in lower left back tooth region of mouth since 1 month. On clinical examination grossly decayed mandibular first molar was observed. Tenderness on vertical percussion was present i.r.t 36. The treatment plan advised was non-surgical root canal treatement i.r.t. 36. On radiographic examination periapical lesion was associated i.r.t. 36. The working length was confirmed radiographically using #15 K-file. Coronal flaring was done using Sx (Protaper Gold File System. The remaining root canal system was prepared with rotary file system using Protaper Gold File System till F2 with copious irrigation using 5.25% sodium hypochloride solution. Mastercone selection was done using 25.06 guttapercha. The canals were dried with paper points and obturated by laterally condensed guttapercha (Roeko, Germany) root canal sealer. The treatment was completed in 2 visits. The post endodontic restoration was done using RibbondFibers, the GP was sheared till 2-3 mm below the canal orifice in mesiobuccal, mesiolingual and distal canals. The cut sections of ribbondfibers were placed vertically in each canal and cured. The core build up was done using flowable and packable composite, followed by tooth preparation to receive a PFM prosthesis irt 36.
The primary objective in endodontic therapy is complete obturation of root canal space to prevent reinfection.
Management of immature root with a necrotic pulp and apical periodontitis is a challenging task. The infected root canal space cannot be disinfected with the standard protocol. Obturation of the root canal is difficult because of lack of apical barrier for containing the root filling material. Treatment of choice in such cases is the apexification procedure, i.e., establishing an apical barrier. Calcium hydroxide has been widely used for the induction of hard tissue barrier. 3
Apexification is a form of treatment that involves cleaning of the root canal and filling it with a temporary medication that stimulates the formation of a calcified barrier at the apex, after which, permanent obturation with gutta-percha is done. Favourable results have been obtained after apexification in narrow open apex cases. However, in our patient, the upper central incisor with a wide open apex also showed successful apical barrier formation at the end of one year.
Case 4
A 18-year-old female patient reported with a chief complaint of pain in her upper front tooth region for past two days. Patient gave history of dull throbbing pain for the past 6 months in the same region. Past medical and dental history was non-contributory. Clinical examination showed Ellis Davis Class IV Fracture in upper left central incisor (21). Sensibility test showed no response in 21. Radiographic examination showed blunderbuss canal and a periapical radiolucency in relation to 21. (Figure 1). Based on the clinical examination, sensibility test and radiographic findings, a provisional diagnosis of Ellis Davis Class IV fracture with open apex and periapical pathology was made. Apexification was planned with MTA (PROROOT Densply). A written consent was taken from the patient after explaining the treatment protocol. In the first visit, access opening was done under isolation using endo access bur #1.Canal patency was checked using a #10 K file and working length was determined using Ingle’s Radiographic method.
Biomechanical preparation was done using K files using step back technique. Irrigation was done using 5.25 % NaOCl and saline). Chlorhexidine was used as a final irrigant. Calcium Hydroxide was placed using a Lentulo spiral and tooth was temporized. Patient was recalled after a week. In the second visit, access cavity was re-established, canal was irrigated copiously following the same protocol and dried with sterile paper points.MTA) was mixed according to the manufacturer’s protocol and and packed to a thickness of 5 mm in the apical third using a hand plugger (Figure 1.4). A sterilecotton pellet was placed in the canal and the tooth was temporized. Patient was recalled after two days. In the subsequent visit, obturation was done using thermoplasticized guttapercha and Composite resin restoration was placed to seal the access cavity.
Case 5
A 21-year-old female patient came with a chief complaint of pain in her upper front tooth region for past two days. Patient gave history of dull throbbing pain for the past 6 months in the same region. Past medical and dental history was non-contributory. Clinical examination showed Ellis Davis Class IV Fracture in upper left central incisor (21). Sensibility test showed no response in 21.Radiographic examination showed blunderbuss canal and a periapical radiolucency in relation to 21. Based on the clinical examination, sensibility test and radiographic findings, a provisional diagnosis of Ellis Davis Class IV fracture with open apex and periapical pathology was made. Apexification was planned with MTA (PROROOT Dentsply).A written consent was taken from the patient after explaining the treatment protocol. In the first visit, Access opening was done under isolation using endo access bur #1.Canal patency was checked using a #10 K file and working length was determined using Ingle’s Radiographic method. Biomechanical preparation was done using K files usingstep back technique. Irrigation was done using 5.25 % NaOCl and saline). Chlorhexidine was used as a final irrigant. Calcium Hydroxide was placed using a Lentulo spiral) and tooth was temporized. Patient was recalled after a week. In the second visit, access cavity was re-established, canal was irrigated copiously following the same protocol and dried with sterile paper points. MTA was mixed according to the manufacturer’s protocol and and packed to a thickness of 5 mm in the apical third using a hand plugger. A sterilecotton pellet was placed in the canal andthe tooth was temporized. Patient was recalled after two days. In the subsequent visit, obturation was done using thermoplasticized guttapercha and Composite resin restoration was placed to seal the access cavity. Patient was recalled after a month for follow up.
Case 6
An 31year old female patient reported with a chief complaint of discolored left maxillary central incisor with a history of trauma 10 year back. The concerned tooth did not respond to both electric and heat test. The periapical radiograph revealed a large blunderbuss canal of the same tooth. On clinical examination, Ellis Class I fracture in permanent left maxillary central incisor was evident. Apexification with MTA was planned. Access opening was prepared and working length was determined; irrigation was done with saline. Biomechanical preparation was carried out using 70 size k file with circumferential filing motion. Root canal debridement was done using alternative irrigation with 2.5% NaoCl and saline. Calcium hydroxide was placed in the root canal and patient recalled after 5 days. At subsequent appointment, canal was irrigated with 2.5% NaoCl and 2% chlorhexidine. The canal was dried with paper points and MTA placed with pluggers until thickness of 6 mm. A wet cotton pellet was placed in the canal and access cavity was sealed with temporary cement. In next appointment, root canal was obturated with using lateral condensation technique. Access cavity sealed with glass ionomer cement.
Conclusion
According to a study (Ramesh et al. 2016) on assessing the mode of failure following load application, it was observed that the Ribbond post system exhibited 100% of repairable failures in all the specimens. On the other hand, the fibre post group had 83.3% of repairable failures which was significantly lower than the Ribbond group. The fracture patterns did not have any influence on the mode of failure in both the post systems. Both the post systems compared in this study were fibre-reinforced composite posts having similar modulus of elasticity to that of dentin. The lower flexural modulus of fibre-reinforced posts can decrease the incidence of root fracture. It was observed that unlike Ribbond group, the Reforpost group exhibited a few modes of ‘non-repairable failures’. The fact that Ribbond produced a majority of repairable failures is in accordance with other studies conducted. 2
Ozcopur et al. showed that individual posts such as Ever Stick and Ribbond showed more repairable fracture modes when compared to a prefabricated fibre post, UniCore, and a metal post, Para Post.4 Another in vitro study on the fracture resistance and the incidence of vertical root fracture of pulpless teeth restored with various post-and-core systems found that the polyethylene woven fibre (Ribbond) and composite resin without a prefabricated post resulted in significantly fewer vertical root fractures, but mean failure load was the lowest.5 Aggarwal et al. also reported that Ribbond exhibited 100% repairable failure modes, similar to what was noted in the present study, thus proving Ribbond to be a favourable restorative modality. 6
Teeth with immature root apex are usually treated surgically or a combination of non-surgical and surgical retreatment is employed. However, patients are sometimes unwilling to be subjected to a surgical procedure. The apical barrier technique that is used for apical closure of immature teeth with necrotic pulps may be an alternative to surgical approach.
Apart from immature teeth with necrotic pulps, there are cases of mature teeth with complete root formation that need to be treated with an apexification technique as there is a lack of apical constriction. This may be due to apical resorption, perforation, over-instrumentation or failed apicoectomy without placement of a retrofilling.7
According to a study (S. Stefopoulos et al. 2012) Favorable results have been demonstrated for non-surgical retreatment of teeth with failed surgeries and amalgam root-end fillings, after orthograde removal of the retrofillings and placement of MTA apical plug. The use of white MTA as an apical barrier to successfully retreat a failed apicectomy was demonstrated in this study.8