- Visibility 138 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijce.2023.027
-
CrossMark
- Citation
Perio-scopy– A literature review
- Author Details:
-
Neera Ohri
-
Sonia Godara *
-
Bharat Rao
-
Rohan Gupta
Introduction
A Perioscope is a dental endoscope (endo means “within” and scope means “observe or look at”), and the procedure using this tool is known as Perioscopy. It is used to view inside the pockets between the gum and teeth at high magnifications.[1]
The World Health Organization indicated that tooth loss caused by severe periodontitis occurs in 15%–20% on middle-aged adults (35–44 years old) in most populations worldwide. [2]
Traditional Periodontal Therapy was based on the concept of debridement of the tooth and root surfaces by removing the plaque bio-films and calculus deposits by manual and powered scalers and root planinginstruments. This procedure to reduce the bacterial load of the sub gingival environment was done by either using tactile sensation in closed pockets or under direct visualization of the root surfaces by flap surgery.
The efficacy of this treatment was subject to various factors like the subgingval access, root morphology, defect extent and the tactile skills of the periodontist. Brayer et al and Sherman et al have demonstrated that manual mechanical debridement is not a fool proof method and some residual root deposits remain even after periodontal treatment. [3], [4]
The idea of having fibre-optic devices at the end of diagnostic and therapeutic instruments is not new to the field of medicine as medical specialties for the past twenty years have extensively used these kind of fibre-optics to reach inaccessible anatomic locations and done on-invasive surgery. But the adaptation of these kind of fibre-optics to dentistry is relatively new. Especially in the field of periodontics where the inherent limitations like the visual and physical access to the disease involved site of the periodontal pocket may be solved by the introduction of such fibre-optic technologies to the periodontal instruments small enough to enter even into the deepest, most inaccessible pocket in a less invasive way.
This recent concept of using magnification under direct visualization and instrumentation with miniaturized armamentarium is now known as micro-dentistry. [5]
The device used, called a perio-scope uses this fibre-optic technology to illuminate the periodontal pocket offering a clear and magnified view of the root surface and Inaccessible areas such as trifurcations and bi-furcations. The Perioscope can also be used to detect sub gingival calculus remnants, ulcerated sulcular epithelium, cemental perforations and the tortuous pathways of draining sinuses.
Perioscope
This endoscope for dental puposes is manufactured by dental view inc., lake forest CA, USA ([Figure 1]).
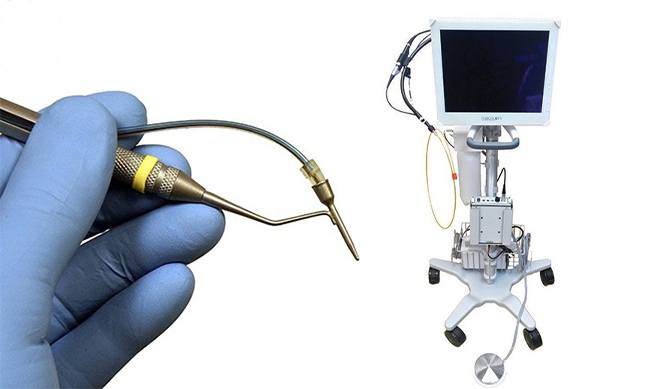
The miniature camera is attached to the fiber. The endoscope has a flexible design that can be combined with other dental instruments. [6]
The use of this technology has been previously described in few case reports and other clinical studies. [7]
The equipement consist of gradient index of lens that is mounted on the end of a 2 m long fused fiber-optic bundle containing 10000 individual light guiding fibers (pixels). Surrounding the fused bundle and lens are 15 large core plastic fiber optic stands for carrying illuminative lights from a remote lamp to the operative site 0.85 mm diameter of flexible plastic tube at the distal end. A spring activated connector located 1mm from the distal end to window sheath.
Armamentarium
The Fiber-Optic Strand
The Sterile Sheath
The Peristaltic Pump
The CCD Camera
The Micro-Surgical Instruments
Indications for perio-scopy
Any periodontal condition with a probing pocket depth (PPD >4) of more than 4mm will benefit from endoscopic visualization and treatment.
The primary benefit of Perioscope is the magnified visualization of the sub gingival calculus attached to the root surfaces which can be debrided with special miniaturized periodontal micro-surgical instruments.
Aberrant root malformations and anatomical variations can be visualized and tracked along their paths and finally restored without any recurrence.
Indications for major periodontal surgery by open access flaps with all its resultant sequelea of recession and root exposure is avoided by microsurgery.
Teeth with a diagnosis of Refractory Periodontal disease and those with chronically inflamed pockets and increasing pocket depths are ideal candidates forperiodontal endoscopy-aided therapeutic procedures.
Teeth with poor prognosis and minimal access to defects under furcations can now be managed with less invasive instrumentation by using periodontal microsurgery improving their treatment outcomes.
Avoiding second surgical procedures in implant mucositis and peri-implantitis by micro-visualization and debridement of diseased implant surfaces plays a positive role in early resolution of the peri-implant infection.
Patients where periodontal surgery is contraindicated due to their medically compromised health status benefit from Perioscopy.[8]
Finally long term treatment outcomes are improved with the use of the least invasive procedures which reduce trauma to healthy surrounding tissues while treating the disease effectively.
Perio-scopy procedure
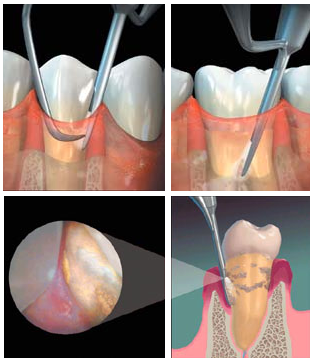
There is very little discomfort during a Perioscopy appointment so while most patients can be treated without anesthesia. Full mouth treatment averages between 90-120 minutes for moderate to advanced periodontitis but these times are based on a dental professional who is highly efficient with a Perioscope. Using the LCD screen the periodontist can see the magnified root surface at a 24x to 48x magnification and approximately 3mm of the root is viewed at one time.
The Perioscope is held in the clinician's left hand (assuming he or she is right handed) while the debridement instrument is manipulated with the right hand. At the end of the Scaling and root planning procedure the results are less damaging to the root surface as the Perioscope allows the periodontist to directly view the calculus deposits instead of solely relying on tactile sensation.
|
Disadvantages |
Advantages |
|
• Learning curve |
• Provides minimally invasive therapy |
|
• Equipment purchase/cost of technology |
• Allows for simultaneous treatment and diagnosis |
|
• Limited availability for instruction |
• Less morbidity than open –flap surgery |
|
• Disruptive technology |
• Less recession and sensitivity than traditional surgical intervention. |
|
|
• Microvisual technology enhances visualization and illumination of treatment site. |
|
|
• May be used by dentist or dental hygienist |
|
|
• No need of assistant during treatment |
|
|
• Can be less expensive than surgery |
|
Anatomical Considerations |
Instrument Access |
|
• Small mouth |
• Narrow, deep pockets |
|
• Muscular tongue |
• Curved roots |
|
• Tight cheeks and lips |
• Close root proximity |
|
• Patients prone to gagging |
• Over – contoured restorations |
|
• Patient cooperation |
• Distal aspects and furcations of maxillary second or third molrs |
|
|
• Narrow furcations and some class III furcations |
Perioscopy in Periodontal Disease
Armitage and Christie in a SEM study in 1973 reported that teeth involved in unresolved and aggressive forms of periodontitis exhibit cemental abnormalities particularly at the cemento-dentinal junction. [9]
Yammaamato in 1999 concur with their findings and added that such periodontal diseased root surfaces have extensive resorption lacunae that characterize the entire length of the root surface. [10]
Poppe et al 2014, carried out a comparative study using periodontal endoscope and periodontalprobe to evaluate the amount of pain reported by patients after detection of calculus. Conducted in-vivo, randomized, split- mouth design comparative study on 30 subjects to assess the amount of pain experienced by patients with 5-8mm pocket depths with atleast 4 sites, after tactile examination of calculus with periodontal endoscope and periodontal probe. Further, quadrants were assigned randomly for tactile examination of calculus with periodontal probe and the other for Periodontal endoscope. The Heft-Parker Visual Analogue Scale (VAS) was used to record subjects‟s pain experience, owing to its ability to measure pain on a continuum along with its validity, reliability and sensitivity. The authors thus concluded statistically significant differences were found in pain perception of patients who had undergone tactile examination of calculus with Periodontal endoscope when compared with periodontal probe. [11]
A study conducted by Geisenger et al 2007 to evaluate residual calculus percentage in single rooted teeth after the extraction. The teeth were divided into two groups and were treated with hand instruments and ultrasonic instruments respectively. After subgingival debridement, the teeth were assessed with an explorer or a periodontal endoscope. The microscopic examination showed, higher percentage of residual calculus on root surfaces that were assessed with an explorer compared with an periodontal endoscope. The difference was statistically significant only when interproximal sites >6mm and buccal sites >4mm were assessed. The authors thus concluded that the subgingival sites assessed with periodontal endoscope shows less percentage of residual calculus when compared with explorer alone. [12]
These findings have implications for the refractory nature of periodontal disease and the clinicaldiagnosis and management of such patients may be made easier by the use of Perioscopy. [13]
Detection and removal of subgingival calculus
Dental calculus primarily consists of inorganic content, including dicalcium phosphate dehydrate, octacalcium phosphate substituted hydroxyapatite, and magnesium-substituted tricalcium phosphate, covered by an unmineralized bacterial layer. The porous structure of calculus largely resembles that of dentin.[10] Kurihara et al, showed that the fluorescence intensity can also be used to distinguish dental calculus from sound enamel with high reproducibility in vitro. [14]
Vedioscope assisted minimally invasive periodontal surgery
Stephen K Harrel et al, reported that, 1 year outcomes from vedioscope assisted minimally invasive periodontal surgery. Sample of 18 patients having a residual pocket probing depth atleast 5mm and 2mm of clinical attachment loss following initial non surgical therapy were treated with V-MIS. There was a statistically significant improvement (p≥ 0.001) in mean PPD (4.11± 0.98 mm) and CAL (4.58±1.19 mm) in surgical site. A mean improvement in the soft tissue also noted (0.48±0.65mm p≥ 0.006). The improvement associated with V-MIS appears to be favour when compare to previous reported result of periodontal regenerative surgery. [15]
Dental implant
The cause of bone loss around implants is unknown, and many different causes for bone loss around implants may exist. Clearly, because the implant interface with the bone is completely different from a natural tooth, it is unlikely that peri-implant bone loss is the same process that occurs in periodontal bone loss around natural teeth.[16]
Surgery is the traditional treatment option for people diagnosed with advanced stages of periodontal disease. Now with perioscopy, for some patients periodontal surgery is not necessary. Perioscopy utilises a miniature dental endoscope with advanced video lighting and 48 times magnification that allows clinicians to see details of tooth anatomy and mineralized deposits and treat periodontal disease in a minimally invasive way.
What is the Treatment Process?
Local anaesthesia will be administered prior to procedure.
A small tip (endoscope) is placed beneath the gingiva.
The endoscope is carefully swept along the tooth root surface removing plaque with water flushing out the pocket.
Fine instruments will be used to remove mineralised bacterial deposits below the gum line.
Once thorough debridement has been achieved, the healing process commences, preventing further gingival damage and tooth loss.
Perioscopy will take a bit longer than the standard appointment due to the intricate nature of the procedure.
Conclusion
The first and foremost consideration for recommending a Perioscope is improved treatment outcomes with greater reductions in probing depths and better root surface attachment gains because a periodontal debridement done under the Perioscope leaves the root surface exceptionally clean and free of infected cementum and calculus which helps the surrounding tissues – the soft tissue wall of the pocket to heal faster and better.
Perioscope is a game changer in the periodontal treatment armamentarium and will revolutionize management of periodontal diseases by becoming the default standard of care for future periodontal procedures.
Conflicts of Interests
The author has no financial interests or conflicts of interests.
Source of Funding
None.
References
- . . . [Google Scholar]
- . WHO Media Centre, The World Oral Health Report (World Health Organization, 2012). . [Google Scholar]
- W K Brayer, J T Mellonig, R M Dunlap, Etal. Scaling and root planing effectiveness: the effect of root surface access and operator experience. JOP 1989. [Google Scholar] [Crossref]
- PR Sherman, LH Hutchens, LG Jewson. The effectiveness of subgingival scaling and root planing. Clinical response related to residual calculus. JOP 1990. [Google Scholar] [Crossref]
- VK Kutsch. Microdentistry: a new standard of care. J Massachusetts Dental Soc 1999. [Google Scholar]
- L Harnack, G Schmitt-Corsitto, J R Gonzales, J Meyle. DentalView DV2 Perioscopy System: an Endoscopic Method for Exploration and Visualization of Subgingival Deposits. Periodontal Pract Today 2004. [Google Scholar]
- V Avradopoulos, RS Wilder, S Chichester, S Offenbacher. Clinical and inflammatory evaluation of Perioscopy on patients with chronic periodontitis. J Dent Hyg 2004. [Google Scholar]
- RV Stambaugh, G Myers, W Ebling, B Beckman, K Stambaugh. Endoscopic visualization of the submarginal gingiva dental sulcus and tooth root surfaces. JOP 2002. [Google Scholar] [Crossref]
- GC Armitage, TM Christie. Structural changes in exposed human cementum. II. Electron microscopic observations. J Periodont Res 1973. [Google Scholar] [Crossref]
- T Yamamoto, T Domon, S Takahashi, N Islam, R Suzuki, M Wakita. The structure and function of the cemento-dentinal junction in human teeth. J Periodont Res 1999. [Google Scholar] [Crossref]
- K Poppe, C Blue. Subjective pain perception during calculus detection with use of a periodontal endoscope. Amn Dent Hygienists' Assoc 2014. [Google Scholar]
- ML Geisinger, BL Mealey, J Schoolfield, JT Mellonig. The effectiveness of subgingival scaling and root planing: an evaluation of therapy with and without the use of the periodontal endoscope. J Periodontol 2007. [Google Scholar] [Crossref]
- P M Bartold, N Ishikawa, Vergel De Dios. . Changing Trends in Periodontal Diagnosis, Disease Recognition & Management 2004. [Google Scholar]
- E Kurihara, T Koseki, K Gohara, T Nishihara, T Ansai, T Takehara. Detection of subgingival calculus and dentine caries by laser fluorescence. J Periodontal Res 2004. [Google Scholar]
- S K Harrel, C M Abraham, F Rivera-Hidalgo, J D Shulman, M E Nunn. Videoscope-Assisted Minimally Invasive Periodontal Surgery: One-Year Outcome and Patient Morbidity. Int J Periodontics Restor Dent 2017. [Google Scholar] [Crossref]
- S K Harrel, Wilson Jr, T G Rivera-Hidalgo, F. A videoscope for use in minimally invasive periodontal surgery. J Clin Periodontol 2013. [Google Scholar]
