Introduction
Noncarious cervical lesions (NCCL) are defined as the loss of dental hard tissue at the cementoenamel junction (CEJ) region without the action of microorganisms or inflammatory processes.1 The etiology of noncarious cervical lesions (NCCL) is considered multifactorial and includes poor oral hygiene practice (behavioural factors),2 consumption of acidic drinks or gastroesophageal reflux, loss of enamel in the areas of stress concentration, parafunctional habits such as bruxism, nail biting, wedging of objects,3 etc. The overall prevalence of tooth wear in the population of the southwest coast of India was highest in the age group 40-60 (63.4%).4 Significantly higher tooth wear was observed in males (45.06%) compared to females (29.19%). The presence of NCCL in the general population of Republika Srpska, Bosnia and Herzegovina revealed that the ratio of male to female patients was 50.9%: 49.1%. The lowest prevalence of NCCL was recorded in the age group of 10 to 25 years and the highest prevalence was found in respondents above 65 years (34.0%).5 Tooth wear was significantly higher in the urban population (44.83%) than in the rural population (29.56%).6
There are numerous restorative treatment modalities for Non carious cervical lesion (NCCL) but due to better adhesive and aesthetic properties as well as mechanical wear resistance,7 conservation of tooth structure composites are generally preferred.8 In composite restorations, hybrid layer plays key role in stability and bond strength of the resin dentin interface. The hybrid layer is a zone where the resin of the adhesive system micromechanically interlocks with dentinal collagen; it contains resin collagen, dentin surface structure and intertubular structure.9
With the passage of time, disintegration of hybrid layer occurs causing deterioration of resin – dentin bond.10 Some of the intrinsic host derived enzymes like matrix metalloproteinases are responsible for disintegration of hybrid layer. 10 MMPs are the group of zinc and calcium dependent enzymes which are trapped within the mineralized dentin matrix. The activation of these endogenous MMPs can lead to the hydrolysis of exposed dentinal collagen and causes degradation of the resin-dentin bond interface.11 MMPs target type I collagen in dentin, causing dentin matrix breakdown. As the collagen in the dentin collapses or degrades, it prevents the penetration of resin into the hybrid layer (Chaussain-Miller et al., 2006; Hannas et al., 2007).12 To counteract the activities of MMPs, different MMP Inhibitors such as chlorhexidine (CHX) (Pashley et al., 2004), chitosan(CH), proanthocyanidin(PAC), and galardin can be used with adhesive system.13 CHX is an antimicrobial agent and also used as disinfectant before the placement of restorations. CHX inhibits MMPs across a broad spectrum and significantly retains the unity of the hybrid layer generated by etch and rinse adhesives. 14 Chitosan has exceptional biological qualities, which include antibacterial capabilities, drug-loading ability, remineralization, and osteogenesis, it is frequently employed in the prevention and treatment of various oral diseases.15 In addition to MMP inhibition activity, chitosan also creates cross-links with dentin collagen to strengthen the fibrils and prevent them from breaking down.16 PACs (proanthocyanidin) are naturally occurring chemicals that have the ability to control the activity of MMPs and has adhesive potential antimicrobial properties which will ultimately reduce nanoleakage and improve the longevity of resinous restoration.
The interface between dentin and the restoration material, as well as the long-lasting strength of the link between them, are of particular interest to researchers. Recently, researchers have profound interest in the interface between dentin and the restorative material. There is scarcity in literature which has evaluated and compared strength of resin composite used to restore NCCLs after its pre-treatment with three different MMP inhibitors used in this study. So present study was carried out with the aim of evaluation of the effect of three different Matrix Metalloproteinase (MMP) inhibitors on flexural bond strength of resin composite restorations; done to restore non carious cervical lesions (NCCL). Null hypothesis was set as there is no effect of surface treatment of NCCL with different MMP inhibitor on flexural bond strength of resin composite used to restore it.
Material and Methods
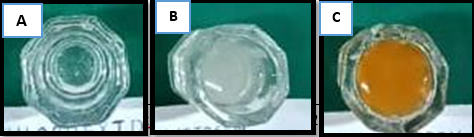
Preparation of 2% Chlorhexidine Di gluconate (Figure 1A)
2% Chlorhexidine Di gluconate – commercially available 2% chlorhexidine in solution (Zodent Safe Plus, Neelkanth Health Care Pvt Ltd)) was used for the study. 17
Preparation of chitosan solution: (Figure 1B)
1.2% Chitosan solution (Meron Marine Hydrocolloids Chullickal Cochin, Kerala, India ISO 22000) with a degree of acetylation >85% was prepared by dissolving 12 mg powder in 100 ml of 1% acetic acid (Sisco Research Laboratories-SRL, Mumbai, India) using a magnetic stirrer (Remi Laboratory Equipment’s, Mumbai, India) for 2h at the rate of 50 rpm at room temperature. 17
Preparation of proanthocyanidin: (Figure 1C)
6.5 g of grape seed extract powder (INLIFE Grape Seed Extract Proanthocyanidins > 95, India) was collected from the capsules and dissolved in 100 mL of distilled water. 17
Sample size calculation: Forty one human premolars were selected for this with following inclusion and exclusion criterias. The sample size was estimated by using the data obtained from a previous study conducted by Gajjela RS et al., (J Conserv Dent. 2017 Mar-Apr; 20(2): 120–124).
Exclusion criteria
Prepared teeth were randomly selected and allotted to each group as follows -
Group I (n = 05) - Etching + Bonding agent + Composite
Group II (n = 12) – Etching + Pre-treatment with CHX + Bonding agent + Composite
Group III (n = 12) – Etching + Pre-treatment with Chitosan + Bonding agent + Composite
Group IV (n = 12) - Etching + Pre-treatment with PA + Bonding agent + Composite.
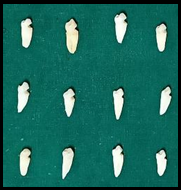
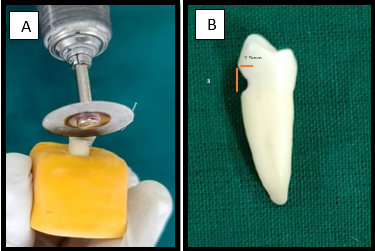
A saucer shaped depression of 2.5 mm depth and 4 mm cervico occlusal length was prepared with bench grinder machine (Figure 2A,B). Prepared surface was smoothened and polished by buffing it for 30 sec to simulate NCCL.
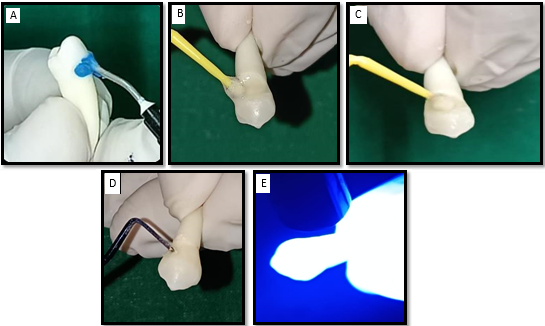
Prepared cavity surfaces in each group (Figure 3, Figure 4, Figure 5, Figure 6) were acid etched with 37% phosphoric acid for 30 sec, rinsed with distilled water for 20 sec and dried with sterile absorbent gauze. Except for Group I (control), prepared surfaces in all other groups (test groups) were pretreated with respective MMP inhibitors for 30 sec and dried with absorbed gauze (Figure 7A-E).
Surface treated prepared surface of NCCL in test groups (group II, III, IV) and untreated prepared surface of NCCL in control group (group I) were restored by applying universal self-etching bonding agent (3M ESPE single bond universal adhesive, St. Paul, MN, USA) and curing it for 20 seconds followed by placement of nanocomposite (Filtek Supreme XTE, colour C4D; 3 M,St. Paul, MN, USA) in incremental manner and curing it for 20 sec each with LED light cure unit (Satelec Mini LED, Acteon Group; light intensity ≥1000 mW/ cm2 according to a Cure Rite Visible Curing Light Meter; Dentsply Caulk) (Figure 7C,D,E). Restorations were finished and polished as per manufacturer’s instructions.
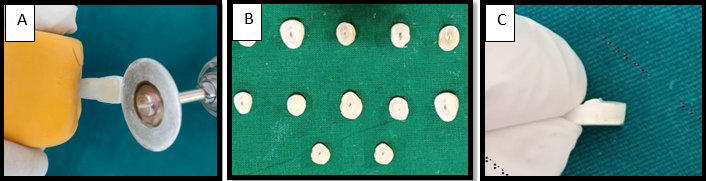
Test specimens were prepared by cutting these teeth transversely at restored NCCL area to form rod shaped samples of 6*3*3 mm (length*width*height). Using a diamond disk (2L x 2W mm, NMD NEXUS MEDODENT, India, C01/220 0.20mm) teeth are sectioned across the adhesive interface with cross-sectional areas of roughly 3mm × 6 mm (Figure 8A-C).
Figure 2
A,B: saucer shaped depression of 2.5 mm depth and 4 mm cervico occlusal legth prepared with bench grinder machine
Flexural bond strength test (Figure 9)
The universal testing machine (ACME Engineers, India. Model No. UNITEST-10Computerized, Software based) was used to load each resin-dentin beam until failure under strain. Two point test with universal testing machine (cross head speed: 1mm/min) was done. Formula for flexural strength use was
Flexural Strength formula: 3PL / 2bd2.,
Where, P: Fracture Load, L: Span between supports, d: Thickness, b: Width
The maximum load at failure divided by the cross-sectional area yielded the flexural bond strength, which was stated in MPa.
Results
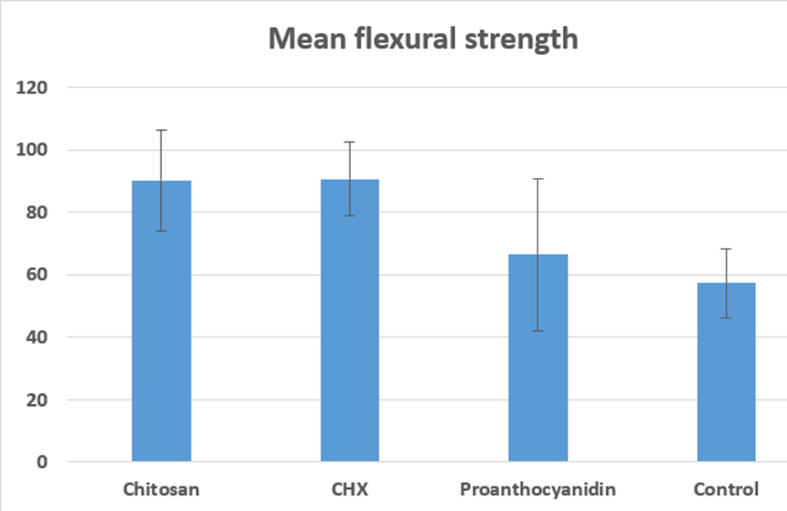
Mean flexural bond strength (MPa) values for different groups are mentioned in Table 1. Chlorhexidine (group II) showed highest mean flexural bond strength followed by chitosan (group III) with statistically insignificant difference (P=1.000) in between them. Proathocyanidin (group IV) showed significantly lower flexural bond strength as compared to group II (P=0.0009) and group III (P=0.011). Control (group I) showed least flexural bond strength. Surface treatment with chlorohexidine and chitosan has found to significantly improve the flexural bond strength of resin composite. Proanthocyanidin showed insignificantly higher flexural bond strength than control (P=0.768) (Table 2) (Figure 10).
Table 1
Flexural bond strength (MPa) among control and test group (One way ANOVA)
|
Group |
Mean (MPa) |
SD |
p-value |
|
Control (group I) |
57.33 |
11.11 |
<0.001* |
|
CHX (group II) |
90.73 |
11.95 |
|
|
Chitosan (group III) |
90.17 |
16.27 |
|
|
Proanthocyanidin (group IV) |
66.41 |
24.35 |
Table 2
Pairwise comparison of flexural bond strength among different groups
Discussion
Through inter- and intramolecular collagen cross-linking, dentin collagen is reinforced and strengthened, increasing the bond strength and stability of the resin/dentin interface over time against enzymatic and/or hydrolytic degradation.
When compared to enamel, bonding to dentin presents a number of difficulties such as Variations in the composition of the substrate, the formation of the hybrid layer, which necessitates demineralizing the dentin collagen matrix in order to allow resin monomers to permeate. Interfacial collagen degradation is caused by the partially exposed collagen in the hybrid layer being susceptible to enzymatic and hydrolytic breakdown.18 The peptide bond on the amino terminal side of glycine (–X-Gly-pro) is hydrolysed by bacterial collagenases, which breaks down collagen.19
According to the literature, exogenous collagen cross-linkage can be created to improve the mechanical characteristics by increasing the number of intra- and intermolecular bonds generated by collagen. Therefore, various collagen cross-linking agents aids in enhancing collagen's mechanical qualities. Bond strength values are found to be increased when these chemicals are used to pre-treat the dentin surface before bonding processes.20
Some of the problems with synthetic cross-linking agents have been solved by a number of naturally occurring cross-linking agents, including proanthocyanidin and genipin. Proline-rich proteins, or PAs, bind to collagen to facilitate the production of new collagen. In addition to coming from a naturally occurring source, it exhibits strong biocompatibility, a quicker rate of reaction than genipin, and its constituents, catechin and epigallocatechin gallate, have been shown to be effective collagenase inhibitors.18
Since genipin discolors easily, it is not an often used medication.Chitosan pretreatment enhanced the mechanical characteristics and resistance to enzymatic degradation of dentin. The cross-linking of chitosan and collagen is facilitated by the intermolecular interaction between positive and negative charged units.21
Hence, the present study, evaluated the effect of pre-treatment of dentin, before acid etching with collagen stabilizing agents such as Chitosan,PA, CHX on the shear bond strength to dentin and microleakage of resin composite at enamel and cemental wall.22
The difference between the coefficient of thermal expansion of the restorative materials and the natural tooth structure results creation of gaps and microleakage at the interface caused by thermally induced strains. Compressed air, neutron activation, electrochemical, fluid filtration, and dye penetration tests are among the in vitro techniques used to investigate microleakage.23
Results of the present study states that group II (CHX) 90.73 MPa and 90.17MPa group III chitosan (CH) showed highest mean flexural bond strength with statistically insignificant diifferance among them. Among test groups, group IV (PA) showed least flexural bond strength (66.41 MPa) insignificantly different from group I (control) (57.33 MPa).
Because chitosan and CHX has more free hydroxyl and amino groups than PA, chitosan group and CHX group exhibited a marginally higher median shear bond strength value. These groups can interact with free reactive groups in chitosan to form chemical bonds with collagen and form cross-links with other reactive molecules. Dentin collagen that has been integrated and cross-linked with chitosan is resistant to deterioration. 19
Because chitosan biopolymers share structural similarities with extracellular matrix components, they facilitate the formation of collagen. In 2011, Shrestha and colleagues postulated that the incorporation of carboxymethyl-chitosan (CMCS) into dentin collagen through photodynamic cross-linking strengthened collagen stabilization by augmenting the quantity of amine reaction sites. This, in turn, led to the creation of ionic complexes between CMCS and collagen, thereby amplifying collagen cross-linking. 21
Conclusion
Within the confines of this in vitro investigation, pre-treatment of the dentin surface with 2% CHX and 1.2% chitosan resulted in a statistically significant increase in the bond strength of resin composite to dentin bonded using a self-etch adhesive as compared with the control group. Therefore, it is safe to suggest that using MMPs as a pre-treatment for dentin can enhance the bonding strength of composite resin to dentin at the chair side.