- Visibility 53 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijce.2024.041
-
CrossMark
- Citation
Management of crown-root fracture encroaching biological width using biodentine
Introduction
Dental injuries are the most common type of facial injuries. The effects of such injuries on teeth can vary widely, from minor enamel chipping to intricate crown-root fractures. A crown-root fracture begins in the crown and extends into the root, affecting the enamel, dentin, and cementum. It accounts for 5% of dental injuries, primarily caused by direct trauma from horizontal or frontal impacts.[1]
Managing a crown root fracture is challenging and completely depends on the extent of the fracture relative to alveolar crest. Pulpal involvement compromises the integrity of the fracture further. When the fracture line extends longitudinally into the sub-gingival area, it interferes with the biologic width. This complicates the management and prognosis of the fracture, as it poses challenges in maintaining periodontal health and ensuring successful treatment outcomes.[2] The commonly employed treatment options in such instances, attempt to expose the fracture line clinically to facilitate the repair of the fractured root surface.[3]
The treatment modalities for crown-root fractures include apically positioned flaps, orthodontic extrusion, and crown lengthening with osteotomy or osseous recontouring where the biologic width is corrected by surgically removing bone away from the restoration margin. Orthodontic extrusion is a time-consuming procedure and may experience relapse due to the stretching of periodontal fibers. [4] Intentional replantation, also referred to as intra-alveolar transplantation, is another method used to treat crown-root fractures. It involves extracting the tooth, repositioning it to a more coronal position, and then splinting it in place. [5]
The biologic width refers to the physiological dimension of the junctional epithelium and connective tissue attachment, typically averaging around 2 mm. [6] This space acts as a barrier against infiltration of bacteria and its by-products. It is crucial not to impinge on this area when restoring a tooth crown for proper periodontal health.[7]
The present case report presents a novel minimally invasive method in the management of a crown-root fracture which was encroaching the biological width, using Biodentine. The advantageous properties of Biodentine, notably its ability to facilitate reattachment and repair, were strategically utilised in this case.
Case Presentation
A 47 year old female patient was referred from Department of Oral and Maxillofacial Surgery with acute pain in maxillary anterior teeth following road traffic accident that occurred one day prior. Immediate composite splinting of 13,12,11,21,22,23 was done to stabilize the mobile teeth on the day of the accident.
On examination
Tooth number 22 had an Ellis class 3 fracture involving mesioincisal and distoincisal angle extending horizontally across the middle third of crown and the hyperplastic pulp was exposed clinically. Periodontal examination showed no signs of periodontal injury and periodontal attachment level appeared to be within normal limits. Radiographic findings did not indicate any root fractures or periapical changes.
A diagnosis of symptomatic irreversible pulpitis secondary to trauma was made and root canal treatment was advised followed by aesthetic correction with composite restoration and crown.
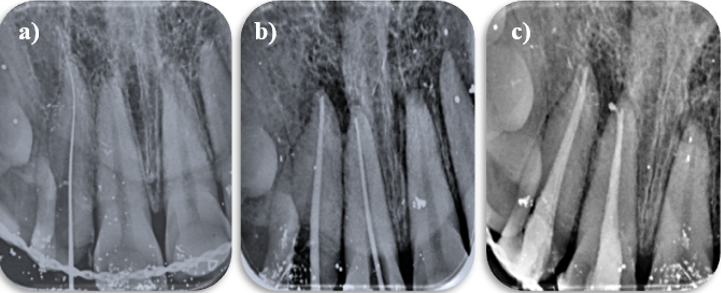
Root canal treatment was initiated under local anesthesia and the hyperplastic pulp was extirpated using a barbed broach. The canal was irrigated using 3% sodium hypochlorite and saline. Working length was estimated using an electronic apex locator (Woodpex III, Woodpecker, Guangxi, China) and confirmed radiographically. Canal cleaning and shaping was done manually upto # 30 (2%) K file ([Figure 1]).
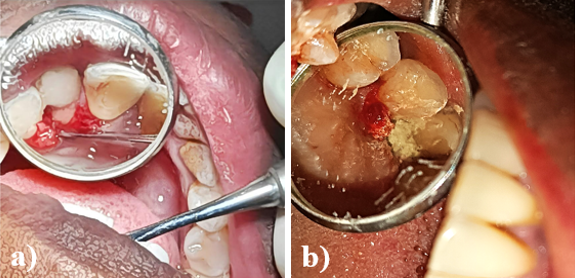
The crown root fracture became evident on cleaning and shaping when a palatal fragment detached from the tooth ([Figure 2]). The loose fragment was removed. The fracture line was seen to extend around 4mm below the free gingival margin, measured using a periodontal probe. For better isolation, visibility of the fracture line, and bleeding control,1mm of the palatal gingiva which was thick and fibrous was removed using laser. The sub crestal extension of the fracture line became evident at this point of time. After obturation of the canal, orthodontic extrusion was suggested to the patient for which she did not comply due to the extended time required for the treatment. Expert opinion from the Department of Periodontics was sought regarding surgical crown lengthening. However, the integrity of the biological width was questionable after crown lengthening. It was then decided to attempt conservative management by building the crown with post and core and composite following which the fractured root would be repaired with Biodentine.


Case was then recalled for post and core treatment after one day. # 3 Peeso reamer (Mani, Tochigi, Japan) was used for post-space preparation, #1.3 fiber post (Tenax, Fiber Trans, Coltene, Whaledent AG, Switzerland) was selected. Post space length was 15mm from the coronal reference point. 5mm gutta percha was preserved apically. Post was luted and core build-up was done using Paracore (Coltene,Whaledent AG, Switzerland) taking care not to extend the material onto the fracture surface below the CEJ. This space however has to be restored to avoid food lodgement and periodontal pocket formation.
Management of root fracture at the palatal aspect
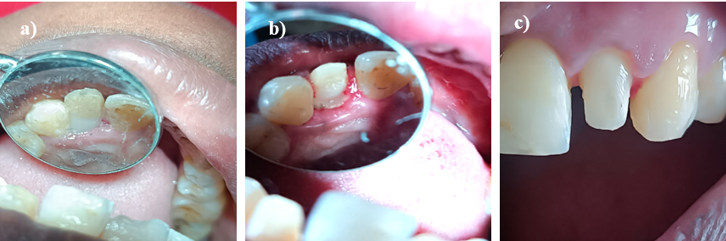
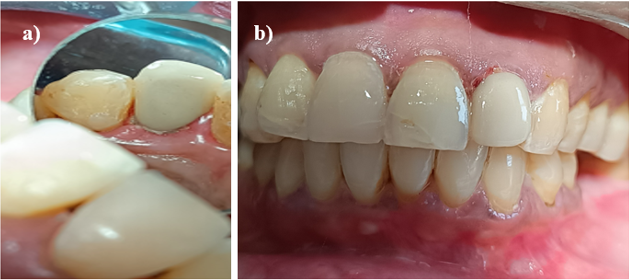
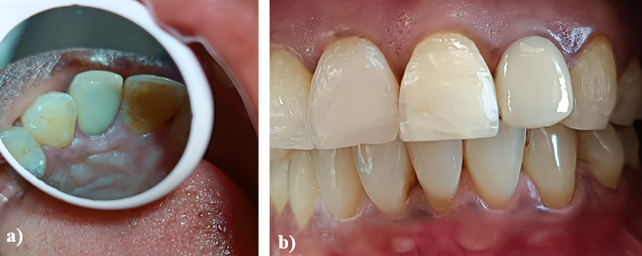
Crevicular incision was placed in relation to 21, 22,23 using # 15 BP blade and flap was reflected using a periosteal elevator ([Figure 3]a) to reveal the subgingival fracture surface. It was seen to extend below the alveolar crest by 4mm. Biodentine (Septodont, Maharastra, India) was mixed according to manufacturer’s instructions and used to cover the fractured surface approximately 2mm thick ([Figure 3]b). Following the placement of Biodentine, flap was apposed using vicryl 4-0 (Ethicon, Mumbai, India) absorbable suture. After one week patient was recalled for tooth preparation, for a porcelain fused metal (PFM) crown ([Figure 4]). Good gingival healing was noted. The periodontal attachment was regained and the gingival sulcus depth was within normal limits. The crown was delivered the following week ([Figure 5], [Figure 6]). Adjacent tooth fracture was also restored with composite.
The patient was recalled at three months intervals to monitor progress. The [Figure 7], depict one year follow up images, demonstrating successful outcomes with no signs of mobility or periodontal pocketing.
Discussion
Subgingival crown fractures present considerable challenges for coronal rehabilitation. The location of the fracture line in affected teeth impacts both the available treatment options and the prognosis. A common dilemma in dentistry is whether to restore a compromised tooth or to extract it and replace it with an implant-supported restoration. [8]
The root length of a fractured incisor needs to maintain a minimum crown-to-root ratio of 1:1 to ensure adequate support for the tooth during normal function [9] which was maintained in the present case.
Bioceramic materials have revolutionized endodontics, greatly improving the prognosis of previously challenging cases. Biodentine, a bioactive calcium silicate-based cement, has been introduced as a dentin substitute. This bio-smart material actively infiltrates exposed dentinal tubules, crystallizing and interlocking with the dentin to enhance its mechanical properties. [10]
Biodentine, a bioactive material, is especially significant for its effects on cementogenesis and osteogenesis. Research indicates that Biodentine boosts osteoblastic differentiation by elevating alkaline phosphatase enzyme activity and fostering the development of calcific nodules in osteoblastic cells, thereby markedly improving mineralization. Additionally, Biodentine has been shown to suppress osteoclastic differentiation and tartrate-resistant acid phosphatase activity in macrophages, which helps to decrease resorption. [11]
Studies conducted by F. Tirone et al. on the effect of Biodentine on the periodontium demonstrated that Biodentine causes less harm to the periodontal ligament. [12]
Research conducted by Duaa Abuarqoub et al., indicated that Biodentine promotes the differentiation of periodontal ligament stem cells at both the cellular and molecular levels, potentially facilitating periodontal regeneration and the reattachment of fibers. Additionally, gingival cells adhere directly to the surface of Biodentine and spread across its surface. [13], [14]
Several studies suggest that Biodentine exhibits potent antibacterial and antifungal properties, which are attributed to its high pH of 12.5. [15]
Biodentine offers distinct advantages over MTA due to the presence of a setting accelerator, calcium chloride, which results in faster initial (6.5 to 16 minutes) and final (13 to 38 minutes) setting times. This accelerated setting not only improves its handling properties but also enhances its strength. During the setting process, Biodentine exhibits a significant increase in compressive strength, reaching 100 MPa within the first hour, 200 MPa at 24 hours, and continuing to strengthen over several days, ultimately reaching 300 MPa after one month. This level of strength is comparable to natural dentine (297 MPa), making Biodentine a promising choice for various dental applications. [16]
According to a study by Grech L et al., Biodentine exhibited the highest compressive strength among the tested materials, attributed to its use of a low water/cement ratio. [17]
In a study by Zhou H et al., the cytotoxicity of Biodentine was compared with that of white MTA and GIC using human gingival fibroblasts. It was observed that Biodentine elicited a similar cellular response to white MTA, and both materials were found to be less cytotoxic than GIC. [14]
Conclusion
Effective minimally invasive management of a complex crown-root fracture in a permanent maxillary lateral incisor using Biodentine has been successfully documented. The success of this treatment depends on the patient's commitment to maintaining excellent oral hygiene practices. Regular and thorough follow-up is crucial to monitor the progress and ensure long-term success. This ongoing observation helps in promptly addressing any complications or issues that may arise, ensuring that the treatment remains effective over time.
Conflict of Interest
None.
Source of Funding
None.
References
- JO Andreasen, FM Andreasen. . Textbook and color atlas of traumatic injuries to the teeth 1994. [Google Scholar]
- GS Bittencourt, FX Almeida, A Rold. Intentional replantation with tooth rotation as indication for treatment of crown-root fractures. Braz J Dent Traumatol 2009. [Google Scholar]
- . Guide AD. Treatment Options for the Compromised Tooth. American endodontics association. 2011. [Google Scholar]
- B Yüzügüllü, Ö Polat, M Üngör. Multidisciplinary approach to traumatized teeth: a case report. Dent Traumatol 2008. [Google Scholar]
- U Tegsjo, H Valerius-Olsson, K Olgart. Intra-alveolar transplantation of teeth with cervikal root fractures. Swed Dent J 1978. [Google Scholar]
- AW Gargiulo, FM Wentz, B Orban. Dimensions and relations of the dentogingival junction in humans. J Periodontol 1961. [Google Scholar]
- JW Robbins. Tissue management in restorative dentistry. Funct Esthet Restor Dent 2007. [Google Scholar]
- A Artieda-Estanga, P Castelo-Baz, A Bello-Castro, I Ramos-Barbosa, B Martin-Biedma, J Blanco-Carrion. Management of a crown-root fracture: A novel technique with interdisciplinary approach. J Clin Exp Dent 2018. [Google Scholar]
- SH Kim, VA Tramontina, V Papalexiou, SM Luczyszyn, MB Grassi, MF Scarpim. Rapid orthodontic extrusion using an interocclusal appliance for the reestablishment of biologic width: a case report. Quintessence Int 2011. [Google Scholar]
- Ö Malkondu, M K Kazandağ, E Kazazoğlu. A review on biodentine, a contemporary dentine replacement and repair material. Biomed Res In 2014. [Google Scholar] [Crossref]
- S Rajasekharan, LC Martens, RG Cauwels, RM Verbeeck. BiodentineTM material characteristics and clinical applications: a review of the literature. Eur Arch Paediatr Dent 2014. [Google Scholar]
- F Tirone, S Salzano, A Piattelli, V Perrotti, G Iezzi. Response of periodontium to mineral trioxide aggregate and Biodentine: A pilot histological study on humans. Aust Dent J 2018. [Google Scholar]
- D Abuarqoub, N Aslam, R Zaza, H Jafar, S Zalloum, R Atoom. The Immunomodulatory and Regenerative Effect of BiodentineTM on Human THP-1 Cells and Dental Pulp Stem Cells. Biomed Res Int 2022. [Google Scholar] [Crossref]
- HM Zhou, Y Shen, ZJ Wang, L Li, YF Zheng, L Häkkinen. In vitro cytotoxicity evaluation of a novel root repair material. J Endod 2013. [Google Scholar]
- V Bhavana, KP Chaitanya, P Gandi, J Patil, B Dola, RB Reddy. Evaluation of antibacterial and antifungal activity of new calcium-based cement (Biodentine) compared to MTA and glass ionomer cement. J Conserv Dent 2015. [Google Scholar]
- M Kaur, H Singh, J S Dhillon, M Batra, M Saini. MTA versus Biodentine: review of literature with a comparative analysis. J Clin Diagn Res 2017. [Google Scholar]
- L Grech, B Mallia, J Camilleri. Investigation of the physical properties of tricalcium silicate cement-based root-end filling materials. Dent Mater 2013. [Google Scholar]
