Introduction
Meticulous treatment of the entire root canal system mandates the result of endodontic interventions. 1 Understanding of anatomical complexities in the root canal system is vital for a successful outcome.2 Failure of endodontic treatment has been attributed to ineffective cleaning and shaping along with inadequate obturation of the canals.3, 4 Also, the inability to identify the presence of a variation may adversely affect its long-term prognosis.5 There are various methods to describe complicated canal configurations which may include examination under a dental operating microscope/magnifying loupe, cone beam computed tomography and micro-computerized tomography other than the presence of an obvious indication on a two-dimensional radiograph.6 The presence of additional canals in the palatal root of maxillary molars has been reported to be 2 to 5.1%. Christie and Thompson et al speculated maxillary molars with two palatal roots may be encountered once every 3 years.7 These extra canals must be identified and debrided to prevent endodontic failure.8 The maxillary molars are typically known to have 4 canals, two mesiobuccal canals (MB and MB2), one distobuccal canal (DB) and one palatal canal (P). The following case report describes the occurrence of an ‘extra’ palatal canal in a maxillary first molar.
Case Report
A 37-year-old female patient reported to the Department of Conservative Dentistry and Endodontics with a chief complaint of pain and food lodgement in the upper right back tooth region since the last 1 month. The patient gave a medical history of Latex allergy along with a previous episode of occurrence of red elevated rashes on contact, no family history was recorded; however, she gave a past dental history of multiple extractions and fillings done in the past. Clinical examination revealed deep mesioproximal caries on tooth no 16 which was tender on percussion, no pain on palpation, no cracks/fractures, no mobility and normal probing depth. Electric pulp test and cold test was performed which did not elicit a response. An intra oral periapical radiograph (IOPA) was advised. The radiograph revealed a coronal radiolucency involving enamel, dentin and approaching pulp with widening of PDL space at the periapex (Figure 1).
Hence a final diagnosis of pulp necrosis with symptomatic apical periodontitis was made and root canal treatment was advised for the same.
Treatment
First appointment
Informed consent was taken from the patient and local anaesthesia 1ml of 2% lignocaine with 1:100,000 adrenaline was administered. Given the patients above mentioned medical history, root canal treatment was carried out using cotton roll isolation. Under 3.3x loupe magnification (Zeiss Eyemag Medical Loupes, Germany), caries excavation was initiated with the help of a large round bur in a high speed airotor handpiece with water coolant. During caries excavation, a ‘drop’ was felt into the pulp chamber following which complete deroofing was performed with the help of an Endo Z bur. Two canals were located in the palatal root, two in the mesiobuccal root (One orifice, two canals) and one in the distobuccal root (Figure 2). The working length was determined with the help of a 15 no K file using an electronic apex locator (Root ZX, J Morita, Japan). Chemo-mechanical preparation was done with the help of Protaper Gold Rotary Files (Dentsply Maillefer, Ballaigues, Switzerland). Both palatal canals were prepared till F3, mesiobuccal (MB and MB2) and distobuccal (DB) canals were prepared till F2. Copious irrigation with 2.5% sodium hypochlorite solution and sterile saline solution was done during instrumentation. Freshly mixed calcium hydroxide paste in chlorhexidine vehicle was placed in all the canals with the help of a lentulospiral. Access preparation was sealed with IRM and the patient was recalled after 10 days.
Second appointment
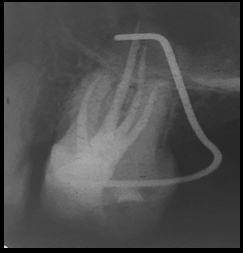
In the second visit, the patient did not exhibit any symptoms and the tooth was no longer tender on percussion. IRM was removed and the canals were irrigated with sterile saline. Once the fit of the master cone was checked, canals were irrigated with 17% EDTA in order to remove the smear layer followed by a final rinse with 2% Chlorhexidine solution. All the canals were dried with the help of absorbent paper points. Obturation was performed using Protaper GP cones (Dentsply Maillefer, Ballaigues, Switzerland) and AH plus sealer (Dentsply DeTrey, Konstanz, Germany) using single cone technique.Post Endodontic Restoration was done with composite (Figure 3).
Discussion
Anatomical complexities are commonly detected in the maxillary first molar. 9 Previous studies have focused mainly on the mesiobuccal root and found to have to have extra canals in 40.3%- 87.2% cases. 10 The palatal root of maxillary molars exhibit these variations as well. Previous studies have reported the incidence of occurrence of an additional palatal canal to be less than 1% . 11 Stone and Stroner et al examined 500 extracted maxillary molars, and concluded that the palatal root had additional canals in <2% of cases. 12 However, Mohara et al reported this occurrence in 0.31% of cases . 13 Usually when supplementary canals exist, modification of the access cavity is required. Particularly, if the orifice of the palatal root canal is eccentrically located, the possibility of an additional canal should be considered. The use of a dental operative microscope/magnifying loupes provides better visualization of the operative field. Without it, the detection of additional canals become unpredictable. Anatomical variations can occur in the palatal root of the maxillary molar, and it is crucial that clinicians are aware of this possibility. With thorough knowledge and appropriate modifications, the clinician can increase the success rate of endodontic treatment.